


Journal of Internal Medicine Concepts & Practice >
Attention to renal damage in rheumatic autoimmune diseases: diagnostic challenges and management strategies
Received date: 2024-11-20
Online published: 2025-10-27
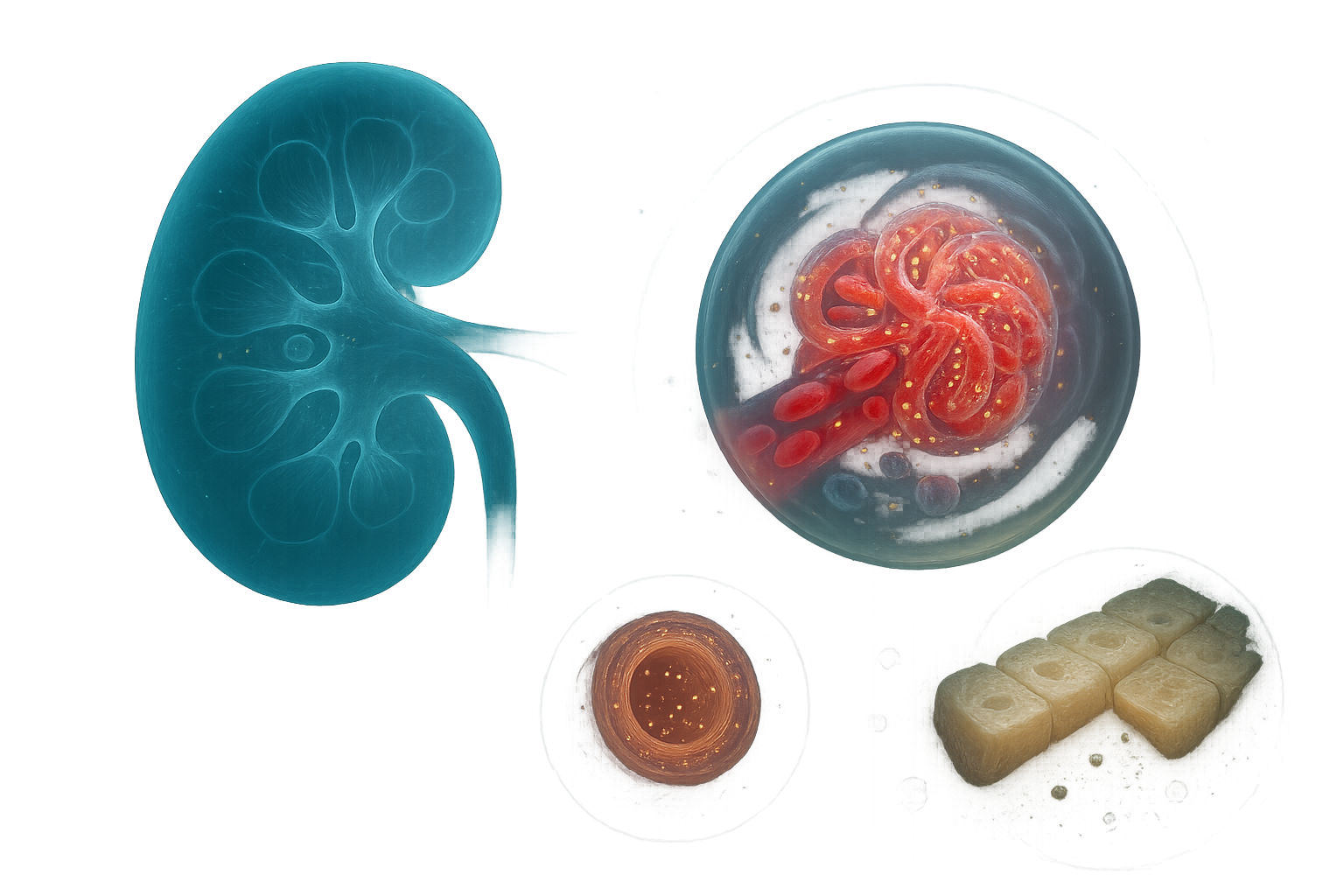
Rheumatic autoimmune diseases often lead to kidney injury, presenting diverse manifestation and complex conditions, ranging from mild proteinuria to severe glomerulonephritis and even renal failure, which has significant impact on patient’s prognosis and quality of life. Because renal damage often has an insidious onset, early diagnosis and intervention are crucial, and development of non-invasive biomarkers is urgently needed. The pathological mechanisms of the disease often involve multiple system; multidisciplinary collaboration including rheumatologists and nephrologists is crucial. The continuous development of biomarkers has made earlier detection and intervention of the disease, bringing new hope for improving patient prognosis. This article discusses the pathogenesis, diagnosis and treatment strategies of renal damage associated with rheumatic autoimmune diseases, emphasizes the importance of multidisciplinary collaboration in disease management. Through precise immunotherapy, appropriate drug adjustments, and kidney protection strategies, the disease can be effectively controlled, and kidney damage can be alleviated and the quality of life of patients will be improved in the future.
LI Huilin . Attention to renal damage in rheumatic autoimmune diseases: diagnostic challenges and management strategies[J]. Journal of Internal Medicine Concepts & Practice, 2025 , 20(04) : 267 -271 . DOI: 10.16138/j.1673-6087.2025.04.01
| [1] | Hill AJ, Thomson RJ, Hunter JA, et al. The prevalence of chronic kidney disease in rheumatology outpatients[J]. Scott Med J, 2009, 54(2):9-12. |
| [2] | Ponticelli C, Doria A, Moroni G. Renal disorders in rheumatologic diseases: the spectrum is changing (Part 1: connective tissue diseases)[J]. J Nephrol, 2021, 34(4):1069-1080. |
| [3] | Kronbichler A, Mayer G. Renal involvement in autoimmune connective tissue diseases[J]. BMC Med, 2013, 11:95. |
| [4] | Mok CC, So H, Hamijoyo L, et al. The 2024 APLAR consensus on the management of lupus nephritis[J]. Int J Rheum Dis, 2025, 28(1):e70021. |
| [5] | Lichtnekert J, Anders HJ. Lupus nephritis-related chronic kidney disease[J]. Nat Rev Rheumatol, 2024, 20(11):699-711. |
| [6] | Jamaly S, Rakaee M, Abdi R, et al. Interplay of immune and kidney resident cells in the formation of tertiary lymphoid structures in lupus nephritis[J]. Autoimmun Rev, 2021, 20:102980. |
| [7] | Siegel CH, Sammaritano LR. Systemic lupus erythematosus[J]. JAMA, 2024, 331(17):1480-1491. |
| [8] | Roveta A, Parodi EL, Brezzi B, et al. Lupus nephritis from pathogenesis to new therapies: An update[J]. Int J Mol Sci, 2024, 25(16):8981. |
| [9] | Parums DV. A review of IgA vasculitis (henoch-sch?nlein purpura) past, present, and future[J]. Med Sci Monit, 2024, 30:e943912. |
| [10] | Ponticelli C, Doria A, Moroni G. Renal disorders in rheumatologic diseases: the spectrum is changing (part 2. Arthridides)[J]. J Nephrol, 2021, 34(4):1081-1090. |
| [11] | Bridoux F, Javaugue V, Nasr SH, et al. Proliferative glomerulonephritis with monoclonal immunoglobulin deposits: a nephrologist perspective[J]. Nephrol Dial Transplant, 2021, 36(2):208-215. |
| [12] | Parisis D, Chivasso C, Perret J, et al. Current state of knowledge on primary Sj?gren’s syndrome, an autoimmune exocrinopathy[J]. J Clin Med, 2020, 9(7):2299. |
| [13] | Vaglio A, Gattorno M, McAdoo S, et al. The kidney in auto-immune and auto-inflammatory processes: definitions, mechanisms, and biomarkers[J]. Front Med (Lausanne), 2023, 9:1129021. |
| [14] | Thurtle E, Grosjean A, Steenackers M, et al. Epidemiology of Sj?gren’s: a systematic literature review[J]. Rheumatol Ther, 2024, 11(1):1-17. |
| [15] | Cole A, Ong VH, Denton CP. Renal disease and systemic sclerosis: An update on scleroderma renal crisis[J]. Clin Rev Allergy Immunol, 2023, 64(3):378-391. |
| [16] | Kamata Y, Sato H, Joh K, et al. Clinical characteristics of biopsy-proven renal sarcoidosis in Japan[J]. Sarcoidosis Vasc Diffuse Lung Dis, 2018, 35(3):252-260. |
| [17] | Patriarcheas V, Tsamos G, Vasdeki D, et al. Antiphospholipid syndrome: A comprehensive clinical review[J]. J Clin Med, 2025, 14(3):733. |
| [18] | Hamadeh M, Boustany S, Fares J. Acute kidney injury following dermatomyositis[J]. Clin Med Res, 2019, 17(3-4):102-104. |
| [19] | Karam S, Haidous M, Royal V, et al. Renal AA amyloidosis: presentation, diagnosis, and current therapeutic options[J]. Kidney Int, 2023, 103(3):473-484. |
| [20] | Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective[J]. Biochem Pharmacol, 2020, 180:114147. |
| [21] | Inker LA, Eneanya ND, Coresh J, et al. New creatinine- and cystatin c-based equations to estimate GFR without race[J]. N Engl J Med, 2021, 385(19):1737-1749. |
| [22] | Alobaidi S, Alotaibi M, Al-Zahrani N, et al. Renal system and rheumatology[M]// Skills in rheumatology. Singapore: Springer, 2021:309-328. |
| [23] | Sawamura M, Sawa N, Yamanouchi M, et al. Use of biologic agents and methotrexate improves renal manifestation and outcome in patients with rheumatoid arthritis: a retrospective analysis[J]. Clin Exp Nephrol, 2022, 26(4):341-349. |
| [24] | Bruschi M, Candiano G, Petretto A, et al. Technology innovation for discovering renal autoantibodies in autoimmune conditions[J]. Int J Mol Sci, 2024, 25(23):12659. |
/
| 〈 |
|
〉 |