

Journal of Surgery Concepts & Practice ›› 2023, Vol. 28 ›› Issue (02): 124-131.doi: 10.16139/j.1007-9610.2023.02.08
• Guideline and consensus • Previous Articles Next Articles
LUO Fangxiu, MA Qianchen, YUAN Fei( )
)
Received:2023-03-22
Online:2023-03-25
Published:2023-06-06
CLC Number:
LUO Fangxiu, MA Qianchen, YUAN Fei. The fifth edition of WHO classification of digestive system tumors: update and progress on biliary system tumors[J]. Journal of Surgery Concepts & Practice, 2023, 28(02): 124-131.
Tab 1
List of tumors of the gallbladder and extrahepatic bile ducts in the fifth edition of WHO classification of digestive system tumors with ICD-O codes
| 分类 | ICD-0 编码 | 分类 | ICD-0编码 |
|---|---|---|---|
| 良性上皮性肿瘤及癌前 病变 | 恶性上皮性肿瘤 | ||
| 胆囊幽门腺腺瘤 | 8140/0 | 胆囊癌 | |
| 胆管上皮内瘤变,低级别 | 8148/0 | 腺癌,NOS | 8140/3 |
| 胆管上皮内瘤变,高级别 | 8148/2 | 肠型腺癌 | 8144/3 |
| 胆囊内乳头状肿瘤伴低级别上皮内瘤变 | 8503/0 | 透明细胞癌,NOS | 8310/3 |
| 黏液腺癌 | 8480/3 | ||
| 胆囊内乳头状肿瘤伴高级别上皮内瘤变 | 8503/2 | 低黏附性癌伴或不伴 印戒细胞 | 8490/3 |
| 胆管导管内乳头状肿瘤伴低级别上皮内瘤变 | 8503/0 | 胆囊内乳头状肿瘤伴 相关浸润性癌 | 8503/3 |
| 胆管导管内乳头状肿瘤伴高级别上皮内瘤变 | 8503/2 | 黏液性囊性肿瘤伴相 关浸润性癌 | 8470/3 |
| 鳞状细胞癌,NOS | 8070/3 | ||
| 未分化癌,NOS | 8020/3 | ||
| 肝外胆管癌 | |||
| 胆管癌 | 8160/3 | ||
| 胆管导管内乳头状肿瘤 伴相关浸润性癌 | 8503/3 | ||
| 鳞状细胞癌,NOS | 8070/3 | ||
| 腺鳞癌 | 8560/3 | ||
| 未分化癌,NOS | 8020/3 | ||
| 神经内分泌瘤,NOS | 8240/3 | ||
| 神经内分泌瘤,G1 | 8240/3 | ||
| 神经内分泌瘤,G2 | 8249/3 | ||
| 神经内分泌瘤,G3 | 8249/3 | ||
| 神经内分泌癌,NOS | 8246/3 | ||
| 大细胞神经内分泌癌 | 8013/3 | ||
| 小细胞神经内分泌癌 | 8041/3 | ||
| 混合性神经内分泌-非神经内分泌肿瘤(MiNEN) | 8154/3 | ||
Tab 2
Characteristics of IPNB
| 特征 | 1型 | 2型 |
|---|---|---|
| 好发部位 | 肝内胆管 | 肝外胆管 |
| 胆管大体特征 | 囊性或圆柱状扩张 | 圆柱形或纺锤状扩张 |
| 黏液分泌 | 常见 | 罕见 |
| 组织学特征 | ||
| 被覆上皮 | 上皮规则、单一,乳头形态>管状形态 | 上皮不规则、复杂,以乳头状形态为主,呈筛状或实性生长模式 |
| 纤维轴心 | 纤细的纤维血管轴心 | 纤细血管,灶性纤维性间质 |
| 组织学亚型 | 胃型、肠型 | 肠型、胰胆管型 |
| 分级 | 多为高级别,伴局灶低级别区域 | 始终是高级别,时有灶性低级别区域 |
| 间质浸润 | 不常见(<50%),多为微小浸润,偶尔呈结节状 | 常见(>80%),呈轻、中程度浸润 |
| 与IPMN相似 程度 | 相似 | 形态多样 |
| 进展可能性 | 较低 | 较高 |
| 预后 | 较好 | 比1型差 |
Tab 3
List of tumors of the intrahepatic bile ducts in the fifth edition of WHO classification of digestive system tumors with ICD-O codes [1]
| 分类 | ICD-0 编码 | 分类 | ICD-0 编码 |
|---|---|---|---|
| 良性胆管肿瘤及癌前病变 | 胆管恶性上皮性肿瘤 | ||
| 胆管腺瘤 | 8160/0 | 肝内胆管癌 | 8160/3 |
| 胆管腺纤维瘤 | 9013/0 | 大胆管型胆管癌 | |
| 胆管上皮内瘤变,低级别 | 8148/0 | 小胆管型胆管癌 | |
| 胆管上皮内瘤变,高级别 | 8148/2 | 胆管导管内乳头状肿瘤伴相关浸润性癌 | 8503/3 |
| 胆管导管内乳头状肿瘤伴低级别上皮内瘤变 | 8503/0 | 黏液性囊性肿瘤伴相关浸润性癌 | 8470/3 |
| 胆管导管内乳头状肿瘤伴高级别上皮内瘤变 | 8503/2 | 未分化癌,NOS | 8020/3 |
| 混合性肝细胞-胆管癌 | 8180/3 | ||
| 黏液性囊性肿瘤伴低级别上皮内瘤变 | 8470/0 | 神经内分泌瘤,NOS | 8240/3 |
| 神经内分泌瘤,G1 | 8240/3 | ||
| 黏液性囊性肿瘤伴高级别上皮内瘤变 | 8470/2 | 神经内分泌瘤,G2 | 8249/3 |
| 神经内分泌瘤,G3 | 8249/3 | ||
| 神经内分泌癌,NOS | 8246/3 | ||
| 大细胞神经内分泌癌 | 8013/3 | ||
| 小细胞神经内分泌癌 | 8041/3 | ||
| 混合性神经内分泌-非神经内分泌肿瘤(MiNEN) | 8154/3 | ||
Tab 4
Pathological characteristics of bile duct cancer in different parts
| 特征 | iCCA | 肝外胆管癌 | |
|---|---|---|---|
| 小胆管型 | 大胆管型 | ||
| 细胞起源 | 肝内小胆管;可能与肝祖细胞有关 | 肝内大胆管或胆管周腺体 | 肝外胆管或胆管周腺体 |
| 形态学 | 被覆立方上皮的小导管状;罕见黏液分泌 | 分泌黏液的柱状细胞形成大导管状或乳头状 | 与大胆管型iCCA类似 |
| 免疫组织 化学表型 | 共同表达CK7、CK19、EMA(MUC1) | ||
| 表达C反应蛋白、N钙黏着素、CD56 | 表达S100、MUC5AC、MUC6、TFF1 | 与大胆管型iCCA类似 | |
| 侵袭性 | 可形成卫星结节 神经、脉管侵犯少见 淋巴结转移少见 | 较少形成卫星结节 神经、脉管侵犯多见 肝内浸润性生长 | 与大胆管型iCCA类似 |
| 分子特征 | IDH1/2、BRCA1/2、BAP1突变,FGFR2融合 | KRAS、TP53突变 | 与大胆管型iCCA类似,KRAS突变频率更高 |
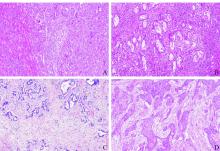
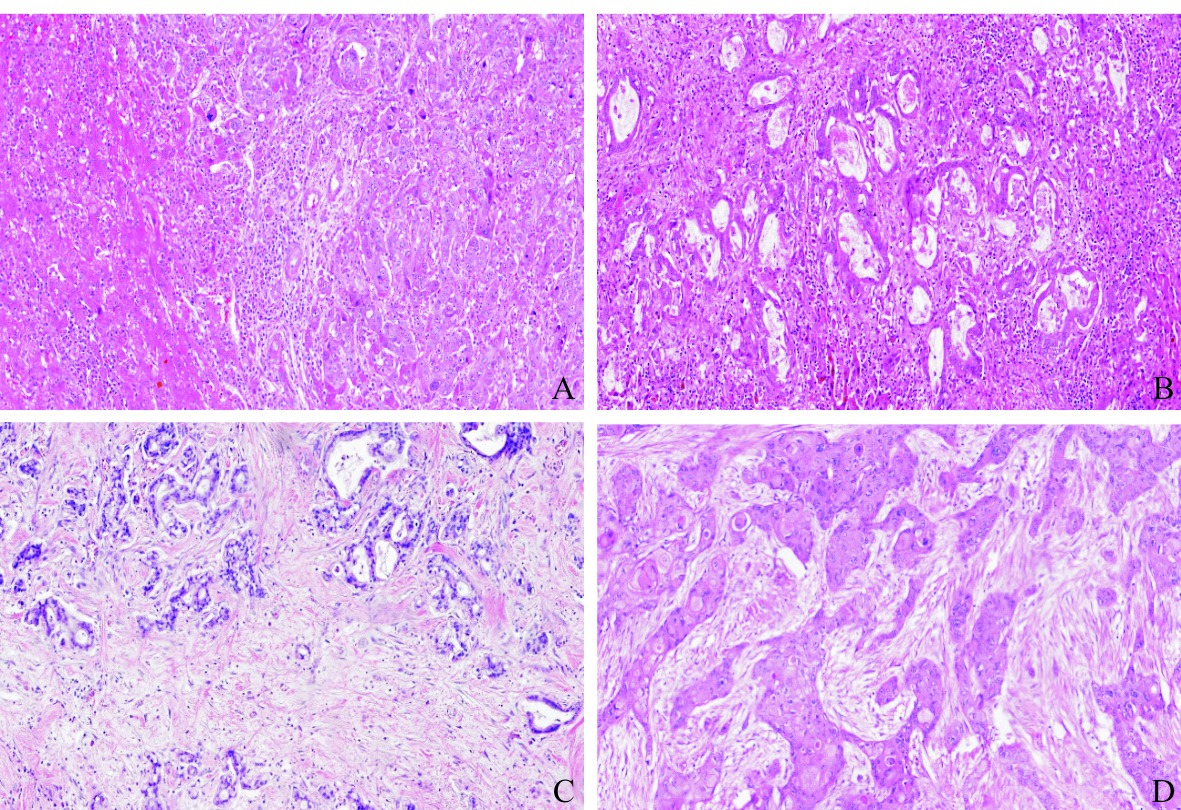
Fig.1
Different histological subtype of cholangiocarcinoma A: Small duct intrahepatic cholangiocarcinoma: cubic cells with no mucin secretion showing small ductal and vesicular components, with solid growth pattern, HE, 100×; B: Large duct intrahepatic cholangiocarcinoma: composed of mucin-secreting tumor cells, forming irregularly expanded glandular ducts with desmoplastic reaction, HE, 50×; C: Extrahepatic cholangiocarcinoma: irregular glands are widely distributed in the stroma of desmoplastic tissue, HE, 100×; D: Hilar bile duct adenosquamous carcinoma: squamous differentiated tumor cells and adenoid cells coexist, HE, 100×.
| [1] | The WHO Classification of Tumors Editorial Board. WHO classification of tumours of digestive system tumors[M]. 5th ed. Lyon:IARC press: 2019. |
| [2] | GERAMIZADEH B. Precursor lesions of cholangiocarcinoma: a clinicopathologic review[J]. Clin Pathol, 2020, 13:2632010X20925045. |
| [3] |
ETTEL M, EZE O, XU R. Clinical and biological significance of precursor lesions of intrahepatic cholangiocarcinoma[J]. World J Hepatol, 2015, 7(25):2563-2570.
doi: 10.4254/wjh.v7.i25.2563 pmid: 26557948 |
| [4] |
HE C, FUKUMURA Y, TORIYAMA A, et al. Pyloric gland adenoma (PGA) of the gallbladder: a unique and distinct tumor from PGAs of the stomach, duodenum, and pancreas[J]. Am J Surg Pathol, 2018, 42(9):1237-1245.
doi: 10.1097/PAS.0000000000001117 pmid: 29975247 |
| [5] |
ADSAY V, JANG K T, ROA J C, et al. Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases[J]. Am J Surg Pathol, 2012, 36(9):1279-1301.
pmid: 22895264 |
| [6] |
ROCHA F G, LEE H, KATABI N, et al. Intraductal pa-pillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas?[J]. Hepatology, 2012, 56(4):1352-1360.
doi: 10.1002/hep.v56.4 URL |
| [7] |
NAKANUMA Y, UESAKA K, KAKUDA Y, et al. Intraductal papillary neoplasm of bile duct: updated clinicopathological characteristics and molecular and genetic alterations[J]. J Clin Med, 2020, 9(12):3991.
doi: 10.3390/jcm9123991 URL |
| [8] |
ALBORES-SAAVEDRA J, ALCÁNTRA-VAZQUEZ A, CRUZ-ORTIZ H, et al. The precursor lesions of invasive gallbladder carcinoma. Hyperplasia, atypical hyperplasia and carcinoma in situ[J]. Cancer, 1980, 45(5):919-927.
doi: 10.1002/(ISSN)1097-0142 URL |
| [9] |
MAZER L M, LOSADA H F, CHAUDHRY R M, et al. Tumor characteristics and survival analysis of incidental versus suspected gallbladder carcinoma[J]. J Gastrointest Surg, 2012, 16(7):1311-1317.
doi: 10.1007/s11605-012-1901-y URL |
| [10] |
BAL M M, RAMADWAR M, DEODHAR K, et al. Patho-logy of gallbladder carcinoma: current understanding and new perspectives[J]. Pathol Oncol Res, 2015, 21(3):509-525.
doi: 10.1007/s12253-014-9886-3 URL |
| [11] | ADSAY N V, KLIMSTRA D S. Benign and malignant tumors of the gallbladder and extrahepatic biliary tract - sciencedirect[M]//ODZE R D, GOLDBLUM J R. Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas. 2nd ed. Philadelphia: W.B.Saunders, 2009:845-875. |
| [12] |
DURSUN N, ESCALONA O T, ROA J C, et al. Mucinous carcinomas of the gallbladder: clinicopathologic analysis of 15 cases identified in 606 carcinomas[J]. Arch Pathol Lab Med, 2012, 136(11):1347-1358.
doi: 10.5858/arpa.2011-0447-OA pmid: 23106580 |
| [13] |
VARDAMAN C, ALBORES-SAAVEDRA J. Clear cell carcinomas of the gallbladder and extrahepatic bile ducts[J]. Am J Surg Pathol, 1995, 19(1):91-99.
pmid: 7802141 |
| [14] |
KONISHI E, NAKASHIMA Y, SMYRK TC, et al. Clear cell carcinoid tumor of the gallbladder - a case without von Hippel-Lindau disease[J]. Arch Pathol Lab Med, 2003, 127(6):745-747.
doi: 10.5858/2003-127-745-CCCTOT URL |
| [15] |
ROA J C, BASTURK O, ADSAY V. Dysplasia and carcinoma of the gallbladder: pathological evaluation, sampling, differential diagnosis and clinical implications[J]. Histopathology, 2021, 79(1):2-19.
doi: 10.1111/his.v79.1 URL |
| [16] |
ROA J C, TAPIA O, CAKIR A, et al. Squamous cell and adenosquamous carcinomas of the gallbladder: clinicopathological analysis of 34 cases identified in 606 carcinomas[J]. Modern Pathol, 2011, 24(8):1069-1078.
doi: 10.1038/modpathol.2011.68 pmid: 21532545 |
| [17] |
TASKIN O C, AKKAS G, MEMIS B, et al. Sarcomatoid carcinomas of the gallbladder: clinicopathologic characteristics[J]. Virchows Arch, 2019, 475(1):59-66.
doi: 10.1007/s00428-019-02583-z |
| [18] |
RIZVI S, KHAN S A, HALLEMEIER C L, et al. Cholangiocarcinoma - evolving concepts and therapeutic strategies[J]. Nat Rev Clin Oncol, 2018, 15(2):95-111.
doi: 10.1038/nrclinonc.2017.157 pmid: 28994423 |
| [19] |
ALBORES-SAAVEDRA J, CHABLÉ-MONTERO F, MÉNDEZ-SÁNCHEZ N, et al. Adenocarcinoma with pyloric gland phenotype of the extrahepatic bile ducts: a previously unrecognized and distinctive morphologic variant of extrahepatic bile duct carcinoma[J]. Hum Pathol, 2012, 43(12):2292-2298.
doi: 10.1016/j.humpath.2012.04.003 URL |
| [20] |
LENDVAI G, SZEKERCZÉS T, ILLYÉS I, et al. Cholangiocarcinoma: classification, histopathology and molecular carcinogenesis[J]. Pathol Oncol Res, 2020, 26(1):3-15.
doi: 10.1007/s12253-018-0491-8 pmid: 30448973 |
| [21] |
NAKAMURA H, ARAI Y, TOTOKI Y, et al. Genomic spectra of biliary tract cancer[J]. Nat Genet, 2015, 47(9):1003-1010.
doi: 10.1038/ng.3375 pmid: 26258846 |
| [22] |
KIM S J, AKITA M, SUNG Y N, et al. MDM2 amplification in intrahepatic cholangiocarcinomas: its relationship with large-duct type morphology and uncommon KRAS mutations[J]. Am J Surg Pathol, 2018, 42(4):512-521.
doi: 10.1097/PAS.0000000000001006 URL |
| [23] |
LOUIS C, PAPOUTSOGLOU P, COULOUARN C. Molecular classification of cholangiocarcinoma[J]. Curr Opin Gastroenterol, 2020, 36(2):57-62.
doi: 10.1097/MOG.0000000000000611 URL |
| [24] |
PUJALS A, AMADDEO G, CASTAIN C, et al. BRAF V600E mutations in bile duct adenomas[J]. Hepatology, 2015, 61(1):403-405.
doi: 10.1002/hep.27133 URL |
| [25] |
PUJALS A, BIOULAC-SAGE P, CASTAIN C, et al. BRAF V600E mutational status in bile duct adenomas and hamartomas[J]. Histopathology, 2015, 67(4):562-567.
doi: 10.1111/his.2015.67.issue-4 URL |
| [26] |
SASAKI M, SATO Y, NAKANUMA Y. Bile duct ade-noma may be a precursor lesion of small duct type intrahepatic cholangiocarcinoma[J]. Histopathology, 2021, 78(2):310-320.
doi: 10.1111/his.v78.2 URL |
| [27] |
ARNASON T, BORGER D R, CORLESS C, et al. Biliary adenofibroma of liver: morphology, tumor genetics, and outcomes in 6 cases[J]. Am J Surg Pathol, 2017, 41(4):499-505.
doi: 10.1097/PAS.0000000000000773 pmid: 28266931 |
| [28] |
GUPTA A, DIXON E. Epidemiology and risk factors: intrahepatic cholangiocarcinoma[J]. Hepatobiliary Surg Nutr, 2017, 6(2):101-104.
doi: 10.21037/hbsn URL |
| [29] | MOEINI A, HABER P K, SIA D. Cell of origin in biliary tract cancers and clinical implications[J]. JHEP Rep, 2021, 3(2):100226. |
| [30] |
MATSUKUMA K E, YEH M M. Update on the pathology of liver neoplasms[J]. Ann Diagn Pathol, 2019, 38:126-137.
doi: S1092-9134(18)30305-8 pmid: 30597357 |
| [31] |
NAKANUMA Y, MIYATA T, UCHIDA T. Latest advances in the pathological understanding of cholangiocarcinomas[J]. Expert Rev Gastroenterol Hepatol, 2016, 10(1):113-127.
doi: 10.1586/17474124.2016.1104246 URL |
| [32] | MONDACA S, RAZAVI P, XU C, et al. Genomic characterization of ERBB2-driven biliary cancer and a case of response to ado-trastuzumab emtansine[J]. JCO Precis Oncol,3:PO.19.00223. |
| [33] |
AISHIMA S, ODA Y. Pathogenesis and classification of intrahepatic cholangiocarcinoma: different characters of perihilar large duct type versus peripheral small duct type[J]. J Hepatobiliary Pancreat Sci, 2015, 22(2):94-100.
doi: 10.1002/jhbp.v22.2 URL |
| [34] |
AKITA M, SAWADA R, KOMATSU M, et al. An immunostaining panel of C-reactive protein, N-cadherin, and S100 calcium binding protein P is useful for intrahepatic cholangiocarcinoma subtyping[J]. Hum Pathol, 2021, 109:45-52.
doi: 10.1016/j.humpath.2020.12.005 pmid: 33321161 |
| [35] |
ROSS J S, WANG K, GAY L, et al. New routes to targeted therapy of intrahepatic cholangiocarcinomas revealed by next-generation sequencing[J]. Oncologist, 2014, 19(3):235-242.
doi: 10.1634/theoncologist.2013-0352 pmid: 24563076 |
| [36] |
LOWERY M A, PTASHKIN R, JORDAN E, et al. Comprehensive molecular profiling of intrahepatic and extrahepatic cholangiocarcinomas: potential targets for intervention[J]. Clin Cancer Res, 2018, 24(17):4154-4161.
doi: 10.1158/1078-0432.CCR-18-0078 pmid: 29848569 |
| [37] |
STEINER P E, HIGGINSON J. Cholangiolocellular carcinoma of the liver[J]. Cancer, 1959, 12(4):753-759.
pmid: 13663020 |
| [38] |
NAKANUMA Y, SATO Y, IKEDA H, et al. Intrahepatic cholangiocarcinoma with predominant "ductal plate malformation" pattern: a new subtype[J]. Am J Surg Pathol, 2012, 36(11):1629-1635.
doi: 10.1097/PAS.0b013e31826e0249 pmid: 23073321 |
| [39] |
NAULT J C, VILLANUEVA A. Biomarkers for hepatobiliary cancers[J]. Hepatology, 2021, 73(Suppl 1):115-127.
doi: 10.1002/hep.v73.s1 URL |
| [1] | XU Haimin, ZHANG Peipei. Comparison of performance between three types of automatic immunohistochemical stainer in pathological diagnosis of breast cancer [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(06): 645-649. |
| [2] | . [J]. Journal of Surgery Concepts & Practice, 2012, 17(03): 262-265. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||