

Journal of Surgery Concepts & Practice ›› 2024, Vol. 29 ›› Issue (02): 170-178.doi: 10.16139/j.1007-9610.2024.02.13
• Original article • Previous Articles Next Articles
LIN Qizhu1, LIU Hongzhi1, HUANG Tingfeng1, FAN Ruilin1, ZHOU Weiping2, ZHENG Shuguo3, LOU Jianying4, ZENG Yongyi1( )
)
Received:2023-06-02
Online:2024-03-25
Published:2024-07-01
Contact:
ZENG Yongyi
E-mail:lamp197311@126.com
CLC Number:
LIN Qizhu, LIU Hongzhi, HUANG Tingfeng, FAN Ruilin, ZHOU Weiping, ZHENG Shuguo, LOU Jianying, ZENG Yongyi. Screening and identification of the beneficiaries of adjuvant chemotherapy based on the prognostic model of intrahepatic cholangiocarcinoma[J]. Journal of Surgery Concepts & Practice, 2024, 29(02): 170-178.
Tab 1
Univariate and multivariate analysis of prognostic factors in the training set
| Univariate analysis | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | |||
| Gender | Woman vs. Man | 0.82 | 0.57-1.19 | 0.3 | ||||
| Age(years) | >60 vs. ≤60 | 0.98 | 0.7-1.37 | 0.897 | ||||
| Smoking history | Yes vs. No | 1.13 | 0.8-1.59 | 0.48 | ||||
| Drinking history | Yes vs. No | 2.26 | 1.51-3.38 | <0.001 | 2.49 | 1.65-3.77 | <0.001 | |
| HBV | Yes vs. No | 1.19 | 0.85-1.67 | 0.304 | ||||
| ECOG score | >2 vs. ≤2 | 1.7 | 1.16-2.49 | 0.007 | 1.46 | 0.98-2.16 | 0.048 7 | |
| CA19-9(U/mL) | >37 vs. ≤37 | 1.79 | 1.22-2.63 | 0.003 | 1.42 | 0.95-2.13 | 0.091 1 | |
| CEA(μg/L) | >5 vs. ≤5 | 1.46 | 0.9-2.37 | 0.128 | ||||
| TBIL(μmol/L) | >20 vs. ≤20 | 0.94 | 0.68-1.31 | 0.725 | ||||
| Blood loss | >400 vs. ≤400 | 1.05 | 0.66-1.69 | 0.828 | ||||
| Blood transfusion | Yes vs. No | 1.4 | 0.8-2.43 | 0.234 | ||||
| Margin(cm) | ≥1 vs. <1 | 0.71 | 0.41-1.21 | 0.205 | ||||
| Method of hepatectomy | Non-anatomical vs. Anatomical | 0.64 | 0.45-0.89 | 0.009 | 0.7 | 0.49-0.99 | 0.042 | |
| LND | Yes vs. No | 1.41 | 0.9-2.19 | 0.132 | ||||
| Lymph node status | N0 vs. Nx | 0.9 | 0.5-1.63 | 0.728 | ||||
| N1 vs. Nx | 3.3 | 1.8-6.03 | <0.001 | 2.6 | 1.36-4.98 | 0.003 9 | ||
| Gross classification | Non-MF(mass forming) vs. MF | 1.31 | 0.94-1.82 | 0.111 | ||||
| Histological classification | Non-adenocarcinoma vs. Adenocarcinoma | 0.47 | 0.21-1.05 | 0.067 | ||||
| Tumor differentiation | Poor vs. Well &moderate | 1.88 | 1.12-3.17 | 0.017 | 2.28 | 1.31-3.95 | 0.003 5 | |
| Number of tumors | Multiple vs. Single | 1.72 | 1.22-2.42 | 0.002 | 1.48 | 1.02-2.14 | 0.038 2 | |
| Tumor maximum diameter (cm) | >5 vs. ≤5 | 1.53 | 1.07-2.21 | 0.021 | 1.37 | 0.94-2 | 0.096 7 | |
| MVI | Yes vs. No | 1.2 | 0.75-1.93 | 0.444 | ||||
| Complications | Yes vs. No | 1.5 | 0.93-2.41 | 0.093 | ||||
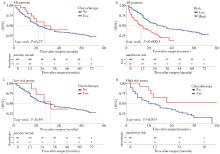
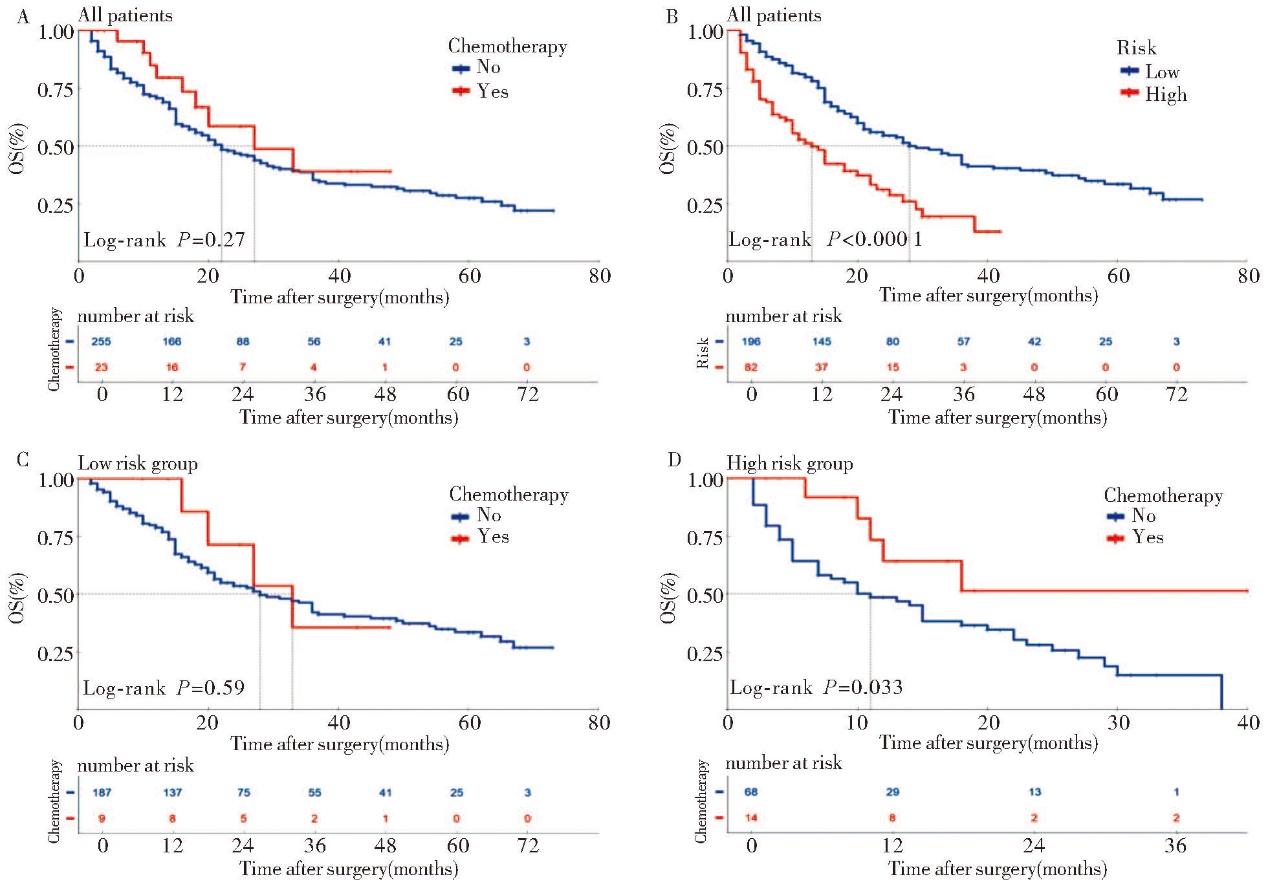
Fig 5
Comparison of survival curves A: Adjuvant chemotherapy and non-adjuvant chemotherapy in the overall cohort; B: Low-risk group and high-risk group in the overall cohort; C: Adjuvant chemotherapy and non-adjuvant chemotherapy in the low-risk group; D: Adjuvant chemotherapy and non-adjuvant chemotherapy in the high-risk group.
Tab 2
Clinical and pathological data in ICC patients afterradical resection with and without adjuvant chemotherapy[n(%)]
| Characteristics | Group | Non- chemotherapy(n=255) | Chemotherapy(n=23) | P value |
|---|---|---|---|---|
| Gender | Man | 165 (64.71) | 15 (65.22) | 1 |
| Woman | 90 (35.29) | 8 (34.78) | ||
| Age (year) | ≤60 | 149 (58.43) | 16 (69.57) | 0.412 5 |
| >60 | 106 (41.57) | 7 (30.43) | ||
| Smoking history | No | 167 (65.49) | 16 (69.57) | 0.868 8 |
| Yes | 88 (34.51) | 7 (30.43) | ||
| Drinking history | No | 206 (80.78) | 22 (95.65) | 0.135 |
| Yes | 49 (19.22) | 1 (4.35) | ||
| HBV | No | 97 (38.04) | 6 (26.09) | 0.362 1 |
| Yes | 158 (61.96) | 17 (73.91) | ||
| ECOG score | ≤2 | 206 (80.78) | 22 (95.65) | 0.135 |
| >2 | 49 (19.22) | 1 (4.35) | ||
| CA19-9 (U/mL) | ≤37 | 190 (74.51) | 10 (43.48) | 0.003 4 |
| >37 | 65 (25.49) | 13 (56.52) | ||
| CEA (μg/L) | ≤5 | 216 (84.71) | 13 (56.52) | 0.001 9 |
| >5 | 39 (15.29) | 10 (43.48) | ||
| TBIL (μmol/L) | ≤20 | 128 (50.20) | 10 (43.48) | 0.689 6 |
| >20 | 127 (49.80) | 13 (56.52) | ||
| Blood loss (mL) | ≤400 | 212 (83.14) | 13 (56.52) | 0.004 6 |
| >400 | 43 (16.86) | 10 (43.48) | ||
| Blood transfusion | No | 220 (86.27) | 17 (73.91) | 0.195 6 |
| Yes | 35 (13.73) | 6 (26.09) | ||
| Margin (cm) | <1 | 184 (72.16) | 3 (13.04) | <0.000 1 |
| ≥1 | 71 (27.84) | 20 (86.96) | ||
| Method of hepatectomy | Anatomical | 103 (40.39) | 11 (47.83) | 0.636 3 |
| Non-anatomical | 152 (59.61) | 12 (52.17) | ||
| LND | No | 201 (78.82) | 7 (30.43) | <0.000 1 |
| Yes | 54 (21.18) | 16 (69.57) | ||
| Lymph node status | Nx | 201 (78.82) | 7 (30.43) | <0.000 1 |
| N0 | 33 (12.94) | 6 (26.09) | ||
| N1 | 21 (8.24) | 10 (43.48) | ||
| Gross classification | MF | 156 (61.18) | 20 (86.96) | 0.025 7 |
| Non-MF | 99 (38.82) | 3 (13.04) | ||
| Histological classification | Adenocarcinoma | 238 (93.33) | 23 (100.00) | 0.410 1 |
| Non-adenocarcinoma | 17 (6.67) | 0 | ||
| Tumor differentiation | Well &Moderate | 225 (88.24) | 12 (52.17) | <0.000 1 |
| Poor | 30 (11.76) | 11 (47.83) | ||
| Number of tumors | Single | 180 (70.59) | 22 (95.65) | 0.019 3 |
| Multiple | 75 (29.41) | 1 (4.35) | ||
| Tumor maximum diameter (cm) | ≤5 | 94 (36.86) | 8 (34.78) | 1 |
| >5 | 161 (63.14) | 15 (65.22) | ||
| MVI | No | 218 (85.49) | 11 (47.83) | <0.000 1 |
| Yes | 37 (14.51) | 12 (52.17) | ||
| Complications | No | 218 (85.49) | 16 (69.57) | 0.088 1 |
| Yes | 37 (14.51) | 7 (30.43) |
| [1] | 中国抗癌协会肝癌专业委员会胆管癌协作组. 原发性肝癌诊疗指南之肝内胆管癌诊疗中国专家共识(2022版)[J]. 中华消化外科杂志, 2022, 21(10):1269-1301. |
| Chinese Society of Liver Cancer Cholangiocarcinoma Cooperative Group. Chinese expert consensus on management of intrahepatic cholangiocarcinoma(2022 edition)[J]. Chin J Dig Surg, 2022, 21(10):1269-1301. | |
| [2] |
BRIDGEWATER J, GALLE P R, KHAN S A, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma[J]. J Hepatol, 2014, 60(6):1268-1289.
doi: 10.1016/j.jhep.2014.01.021 pmid: 24681130 |
| [3] | SINGAL A K, VAUTHEY J N, GRADY J J, et al. Intra-hepatic cholangiocarcinoma—frequency and demographic patterns: thirty-year data from the M.D. Anderson Cancer Center[J]. J Cancer Res Clin Oncol, 2011, 137(7):1071-1078. |
| [4] | MASSARWEH N N, EL-SERAG H B. Epidemiology of hepatocellular carcinoma and intrahepatic cholangiocarcinoma[J]. Cancer Control, 2017, 24(3):1073274817729245. |
| [5] |
GRAVELY A K, VIBERT E, SAPISOCHIN G. Surgical treatment of intrahepatic cholangiocarcinoma[J]. J Hepatol, 2022, 77(3):865-867.
doi: 10.1016/j.jhep.2022.01.004 pmid: 35676107 |
| [6] | CHUN Y S, JAVLE M. Systemic and adjuvant therapies for intrahepatic cholangiocarcinoma[J]. Cancer Control, 2017, 24(3):1073274817729241. |
| [7] | ALTMAN A M, KIZY S, MARMOR S, et al. Adjuvant chemotherapy for intrahepatic cholangiocarcinoma:approaching clinical practice consensus?[J]. Hepatobiliary Surg Nutr, 2020, 9(5):577-586. |
| [8] | QU W F, LIU W R, SHI Y H. Adjuvant chemotherapy for intrahepatic cholangiocarcinoma: far from a clinical consensus[J]. Hepatobiliary Surg Nutr, 2021, 10(6):887-889. |
| [9] | MA K W, CHEUNG T T, LEUNG B, et al. Adjuvant chemotherapy improves oncological outcomes of resectable intrahepatic cholangiocarcinoma:a meta-analysis[J]. Medicine (Baltimore), 2019, 98(5):e14013. |
| [10] | WANG M L, KE Z Y, YIN S, et al. The effect of adjuvant chemotherapy in resectable cholangiocarcinoma:a meta-analysis and systematic review[J]. Hepatobiliary Pancreat Dis Int, 2019, 18(2):110-116. |
| [11] | BÜTTNER S, GALJART B, BEUMER B R, et al. Quality and performance of validated prognostic models for survival after resection of intrahepatic cholangiocarcinoma: a systematic review and meta-analysis[J]. HPB (Oxford), 2021, 23(1):25-36. |
| [12] |
ESNAOLA N F, MEYER J E, KARACHRISTOS A, et al. Evaluation and management of intrahepatic and extrahepatic cholangiocarcinoma[J]. Cancer, 2016, 122(9):1349-1369.
doi: 10.1002/cncr.29692 pmid: 26799932 |
| [13] |
KUBO S, SHINKAWA H, ASAOKA Y, et al. Liver cancer study group of Japan clinical practice guidelines for intrahepatic cholangiocarcinoma[J]. Liver Cancer, 2022, 11(4):290-314.
doi: 10.1159/000522403 pmid: 35978598 |
| [14] | VOGEL A, BRIDGEWATER J, EDELINE J, et al. Bi-liary tract cancer:ESMO clinical practice guideline for diagnosis,treatment and follow-up[J]. Ann Oncol, 2023, 34(2):127-140. |
| [15] | PRIMROSE J N, FOX R P, PALMER D H, et al. Capecitabine compared with observation in resected bi-liary tract cancer(BILCAP):a randomised,controlled,multicentre,phase 3 study[J]. Lancet Oncol, 2019, 20(5):663-673. |
| [16] | EDELINE J, BENABDELGHANI M, BERTAUT A, et al. Gemcitabine and oxaliplatin chemotherapy or surveillance in resected biliary tract cancer (PRODIGE 12-ACCORD 18-UNICANCER GI): a randomized phase Ⅲ study[J]. J Clin Oncol, 2019, 37(8):658-667. |
| [17] | 林起柱, 刘红枝, 周伟平, 等. 术后辅助化疗对肝内胆管癌预后影响的多中心回顾性研究[J]. 中华外科杂志, 2023, 61(4):305-312. |
| LIN Q Z, LIU H Z, ZHOU W P, et al. Effect of postoperative adjuvant chemotherapy on prognosis of patients with intrahepatic cholangiocarcinoma:a multicenter retrospective study[J]. Chin J Surg, 2023, 61(4):305-312. | |
| [18] | WIRASORN K, NGAMPRASERTCHAI T, KHUNTIKEO N, et al. Adjuvant chemotherapy in resectable cholangiocarcinoma patients[J]. J Gastroenterol Hepatol, 2013, 28(12):1885-1891. |
| [19] |
MIURA J T, JOHNSTON F M, TSAI S, et al. Chemotherapy for surgically resected intrahepatic cholangiocarcinoma[J]. Ann Surg Oncol, 2015, 22(11):3716-3723.
doi: 10.1245/s10434-015-4501-8 pmid: 25777092 |
| [20] | SUR M D, IN H, SHARPE S M, et al. Defining the be-nefit of adjuvant therapy following resection for intrahepatic cholangiocarcinoma[J]. Ann Surg Oncol, 2015, 22(7):2209-2217. |
| [21] | REAMES B N, BAGANTE F, EJAZ A, et al. Impact of adjuvant chemotherapy on survival in patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis[J]. HPB (Oxford), 2017, 19(10):901-909. |
| [22] |
TSILIMIGRAS D I, HYER J M, PAREDES A Z, et al. Tumor burden dictates prognosis among patients undergoing resection of intrahepatic cholangiocarcinoma: a tool to guide post-resection adjuvant chemotherapy?[J]. Ann Surg Oncol, 2021, 28(4):1970-1978.
doi: 10.1245/s10434-020-09393-7 pmid: 33259043 |
| [23] | SCHWEITZER N, WEBER T, KIRSTEIN M M, et al. The effect of adjuvant chemotherapy in patients with intrahepatic cholangiocarcinoma:a matched pair analysis[J]. J Cancer Res Clin Oncol, 2017, 143(7):1347-1355. |
| [24] | LI X H, ZHAO C Y, ZHOU E L, et al. Efficacy and safety of adjuvant chemotherapy in T1N0M0 intrahepatic cho-langiocarcinoma after radical resection[J]. BMC Cancer, 2022, 22(1):1159. |
| [25] | 苏敬博, 张景玮, 陈晨, 等. 辅助化疗对肝内胆管癌根治性切除术后患者预后的影响[J]. 中华外科杂志, 2022,(4):356-362. |
|
SU J B, ZHANG J W, CHEN C, et al. Impact of adjuvant chemotherapy on prognosis in intrahepatic cholangiocarcinoma patients underwent radical resection[J]. Chin J Surg, 2022, 60(4):356-362.
doi: 10.3760/cma.j.cn112139-20220110-00021 pmid: 35272427 |
|
| [26] | IZQUIERDO-SANCHEZ L, LAMARCA A, LA CASTA A, et al. Cholangiocarcinoma landscape in Europe: diagnostic,prognostic and therapeutic insights from the ENSCCA registry[J]. J Hepatol, 2022, 76(5):1109-1121. |
| [27] | ENDO Y, MOAZZAM Z, ALAIMO L, et al. Predictive risk-score model to select patients with intrahepatic cho-langiocarcinoma for adjuvant chemotherapy[J]. HPB (Oxford), 2023, 25(2):229-238. |
| [28] | LI Q, ZHANG J, CHEN C, et al. A nomogram model to predict early recurrence of patients with intrahepatic cholangiocarcinoma for adjuvant chemotherapy guidance: a multi-institutional analysis[J]. Front Oncol, 2022,12:896764. |
| [1] | SONG Qingjie, TANG Juanjuan, ZHAO Jianquan, SONG hui, YANG Jun. Effect of hyperlipidemia on prognosis of the patients with hepatitis B related hepatocellular carcinoma [J]. Journal of Surgery Concepts & Practice, 2024, 29(02): 143-147. |
| [2] | DING Jingfeng, AO Weiqun, ZHU Zhen, SUN Jing, XU Lianggen, ZHENG Shibao, YU Jingjing, HU Jinwen. The value of radiomics based on T2WI and DWI of MRI in preoperative prediction of extramural vascular invasion in rectal cancer [J]. Journal of Diagnostics Concepts & Practice, 2024, 23(01): 46-56. |
| [3] | HU Binwei, SHEN Baiyong. Advantages and advances in neoadjuvant therapy of pancreatic cancer [J]. Journal of Surgery Concepts & Practice, 2024, 29(01): 74-80. |
| [4] | LU Zhongxiao, TANG Jie, HUANG Wenhai. Nomogram construction based on SEER and survival prediction of pancreatic cancer patients [J]. Journal of Surgery Concepts & Practice, 2024, 29(01): 46-53. |
| [5] | MO Jiantao, CAO Ruiqi, REN Jiaqiang, GENG Zhimin, WU Zheng, CHENG Yali. Construction of a prognostic Nomogram for patients with incidental gallbladder cancer [J]. Journal of Surgery Concepts & Practice, 2024, 29(01): 40-45. |
| [6] | WANG Shukui, GU Xinliang. Advances in the study of tsRNA as diagnostic and prognostic biomarkers in cancer [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(05): 413-420. |
| [7] | LI Yuefeng, HONG Jin, LI Zhian, RUAN Guodong, CHEN Weiguo. Prognostic analysis of the patients with HER2-positive breast cancer adjuvant treated with trastuzumab: a report of 1 246 cases [J]. Journal of Surgery Concepts & Practice, 2023, 28(05): 469-476. |
| [8] | HU Jingjing, SHEN Yinzhong, LIU Li, LU Hongzhou. Current status and research progress of diagnosis and treatment of AIDS with disseminated non-tuberculous mycobacterial disease [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(04): 402-406. |
| [9] | ZHANG Lanlan, YANG Qiao, NIE Zunzhen, GUO Ying. Thoracic SMARCA4-deficient undifferentiated tumour: a case report [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(04): 389-392. |
| [10] | LIU Yingting, YI Hongmei, WANG Xue, YANG Chunxue, OUYANG Binshen XU Haimin, WANG Chaofu. Clinicopathological features and prognosis of 17 cases of duodenal-type follicular lymphoma [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(04): 362-368. |
| [11] | BAI Yaya, TANG Biwen, HU Yueliang, ZUO Junli, YAO Weiyan. Clinical characteristics and prognosis of eosinophilic gastroenteritis in 71 cases [J]. Journal of Internal Medicine Concepts & Practice, 2023, 18(04): 270-277. |
| [12] | YANG Yi, YANG Xingxia, JIN Sili, ZHANG Xu, ZHU Juanying, CHEN Xiaosong. Clinical application of preoperative MRI examination in breast-conserving surgery for ductal carcinoma in situ [J]. Journal of Surgery Concepts & Practice, 2023, 28(04): 378-382. |
| [13] | BAI Tingting, LI Feika, XU Gang, JIANG Qianwen, WU Fang. A simple prediction model for risk of functional impairment in elderly [J]. Journal of Internal Medicine Concepts & Practice, 2023, 18(03): 177-182. |
| [14] | XU Li, GAO Huajie, YANG Mengge, LI Yue, JI Suqiong. Clinical characteristics of anti-SRP antibody positive immune-mediated necrotizing myopathy with anti-TRIM21/Ro52 antibody positive [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(03): 247-254. |
| [15] | WEI Jian, SUN Jie, CUI Shishuang. Development of a Nomogram model for early diagnosis of Parkinson disease [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(03): 277-282. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||