

诊断学理论与实践 ›› 2023, Vol. 22 ›› Issue (04): 348-361.doi: 10.16150/j.1671-2870.2023.04.004
收稿日期:2023-06-24
出版日期:2023-08-25
发布日期:2023-12-18
通讯作者:
施仲伟 E-mail: Received:2023-06-24
Online:2023-08-25
Published:2023-12-18
摘要:
高血压是一种临床诊断,其定义为血压水平高于某一界值,此时降压治疗的获益明显大于风险。我国目前的高血压诊断标准是诊室收缩压≥140 mmHg和(或)舒张压≥90 mmHg(≥140/90 mmHg)。过去几十年间积累的循证医学,尤其是随机对照试验(randomized controlled trial, RCT)证据显示,高血压患者接受降压药物治疗并使血压降至<140/90 mmHg后,其发生主要心血管事件的风险显著降低。然而,美国2017年美国心脏学院(American College of Cardiology, ACC)和美国心脏学会(American Heart Association, AHA)联合发布的高血压指南(ACC/AHA指南)推荐强化降压,将高血压诊断标准下调至≥130/80 mmHg。我国有专家建议采用这一新标准,但更多的专家指出下调高血压诊断界值,将极大增加慢病管理的负担。2003年,美国高血压指南将糖尿病和慢性肾脏病患者的降压目标下调至<130/80 mmHg,但欧洲专家指出,没有随机对照试验(randomized controlled trial, RCT)支持这种下调能进一步降低主要心血管事件。2014年美国高血压指南得出同样结论,并推荐60岁以下成人(包括糖尿病和慢性肾脏病患者)的降压目标为<140/90 mmHg。新发表的6项RCT显示出不同的结果。皮质下小卒中二级预防试验显示强化降压不能降低卒中后患者的卒中复发率,糖尿病患者控制心血管风险行动试验显示,强化降压不能降低高危糖尿病患者的主要心血管事件发生率。心脏后果预防评价试验-3和中国正常高值血压人群降压治疗试验显示,在中低心血管风险的正常高值血压人群中,降压药物治疗不能减少心血管事件。收缩压干预试验(systolic blood pressure intervention trial,SPRINT)和老年高血压患者血压干预策略试验则显示,强化降压能显著降低主要心血管事件。SPRINT试验是美国ACC/AHA指南下调高血压诊断标准的主要依据,但该试验采用独特的血压测量方法导致血压测值低于常规诊室血压测值。SPRINT试验和老年高血压患者血压干预策略试验均为开放设计、提前终止的研究,且通过停药或减量来升高部分标准治疗组患者血压,这些方法夸大了强化治疗组的获益程度。可见,目前仍然缺乏将高血压诊断界值从140/90 mmHg下调至130/80 mmHg能带来临床获益的高质量证据。
中图分类号:
施仲伟. 从学术角度看高血压诊断界值不应下调至130/80 mmHg[J]. 诊断学理论与实践, 2023, 22(04): 348-361.
SHI Zhongwei. The diagnostic threshold for hypertension should not be lowered down to 130/80 mmhg: an academic perspective[J]. Journal of Diagnostics Concepts & Practice, 2023, 22(04): 348-361.
图2
糖尿病患者强化降压治疗的随机临床试验[33] 横坐标显示试验的英文缩写名称,HOT:高血压最佳治疗试验(Hypertension Optimal Treatment Trial);SHEP:老年收缩期高血压试验(Systolic Hypertension in the Elderly Program);UK:英国前瞻性糖尿病研究(United Kingdom Prospective Diabetes Study);MHOPE:心脏结果预防评价研究微量白蛋白尿、心血管和肾脏结果子研究(Heart Outcomes Prevention Evaluation Study, microalbuminuria, cardiovascular, and renal outcomes substudy);S.Eur:欧洲收缩期高血压试验(Systolic Hypertension in Europe Trial);ABCD-HT:糖尿病适当血压控制研究-高血压患者(Appropriate Blood Pressure Control in Diabetes Study-Hypertensive Patients);ABCD-NT:糖尿病适当血压控制研究-正常血压患者(Appropriate Blood Pressure Control in Diabetes Study-Normotensive Patients);IDNT-IR:厄贝沙坦糖尿病肾病试验-厄贝沙坦组(Irbesartan Diabetes Nephropathy Trial-irbesartan);IDNT-AM:厄贝沙坦糖尿病肾病试验-氨氯地平组(Irbesartan Diabetes Nephropathy Trial-amlodipine);REN:血管紧张素Ⅱ拮抗剂氯沙坦降低非胰岛素依赖型糖尿病患者终点事件研究(Reduction of Endpoints in NIDDM with Angiotensin Ⅱ Antagonist Losartan Study);PROG:培哚普利预防再发卒中研究(Perindopril Protection against Recurrent Stroke Study);ADV:糖尿病和血管疾病患者雅施达和达美康对照评价试验(Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation Trial)。长条图中黄色区域的上下端分别显示常规组和强化组患者在降压治疗后取得的平均收缩压水平。
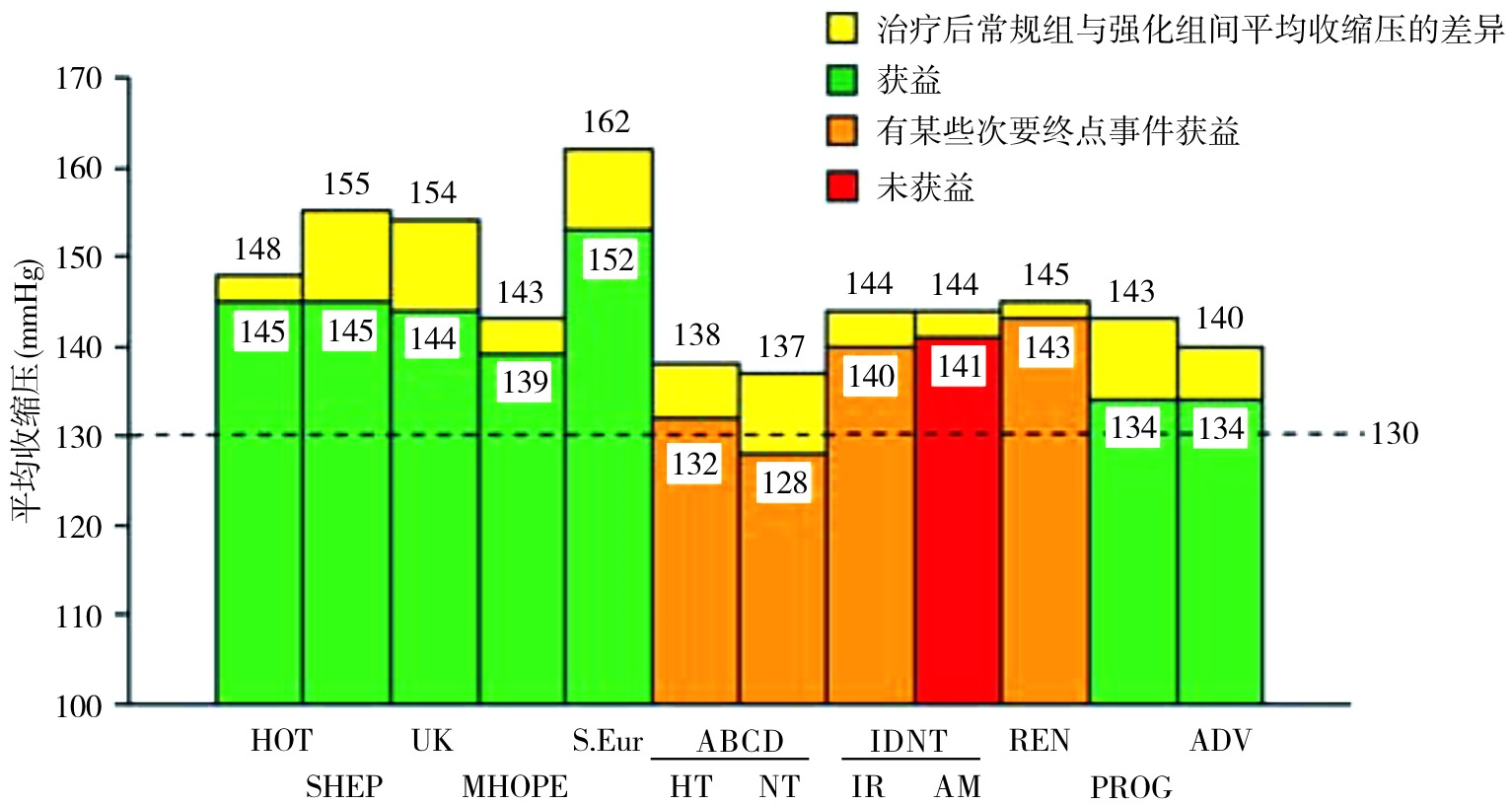
表1
有人在场和无人在场诊室收缩压平均测值的比较[80???-84]
| 作者及国家 | 年份 | 例数 | 诊室收缩压平均值*(mmHg) | ||
|---|---|---|---|---|---|
| 有人诊室测压 | 无人诊室测压 | 血压差 | |||
| Filipovsky,捷克 | 2016 | 353 | 146.9±20.8 | 131.2±21.8 | 15.7±13.8 |
| Agarwal,美国 | 2017 | 275 | 134.5±19.5 | 121.7±17.9 | 12.7±12.0 |
| Bauer,德国 | 2018 | 51 | 135.7±21.5 | 134.2±19.2 | 1.5 |
| Paini,意大利 | 2019 | 329 | 129.8±15.5 | 138.4±16.7 | 8.6±7.7 |
| Cheng,美国 | 2019 | 202 | 145.6±23.5 | 135.3±23.5 | 10.3 |
| [1] | 王薇, 赵冬, 刘静, 等. 中国35-64岁人群血压水平与10年心血管病发病危险的前瞻性研究[J]. 中华内科杂志, 2004, 43(10):730-734. |
| WANG W, ZHAO D, LIU J, et al. A prospective study of relationship between blood pressure and 10-year cardiovascular risk in a Chinese cohort aged 35-64 years[J]. Zhonghua Nei Ke Za Zhi, 2004, 43(10):730-734. | |
| [2] | 曾新颖, 刘世炜, 王黎君, 等. 2013年中国人群血压升高对死亡和期望寿命的影响[J]. 中华流行病学杂志, 2017, 38(8):1011-1016. |
| ZENG X Y, LIU S W, WANG L J, et al. Mortality and life expectancy that attributable to high blood pressure in Chinese people in 2013[J]. Zhonghua Liu Xing Bing Xue Za Zhi, 2017, 38(8):1011-1016. | |
| [3] |
CAO X, ZHAO Z, KANG Y, et al. The burden of cardiovascular disease attributable to high systolic blood pressure across China, 2005-18: a population-based study[J]. Lancet Public Health, 2022, 7(12):e1027-e1040.
doi: 10.1016/S2468-2667(22)00232-8 pmid: 36462514 |
| [4] | 中国高血压防治指南修订委员会, 高血压联盟中国, 中华医学会心血管病学分会, 等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24(1):24-56. |
| Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, et al. 2018 Chinese guidelines for the management of hypertensionWriting Group of 2018[J]. Chin J Cardiovasc Med, 2019, 24(1):24-56. | |
| [5] | 罗兰. 最新发布! 中国高血压诊断标准下调![EB/OL]. 光明网.(2022-11-14) [2023-4-8]. https://m.gmw.cn/baijia/2022-11/14/1303194218.html. |
| LUO L. Latest Release! The diagnostic criteria for hypertension in China have been lowered![EB/OL]. Guangming Net.(2022-11-14) [2023-4-8]. https://m.gmw.cn/baijia/2022-11/14/1303194218.html. | |
| [6] | 钱童心. 中国高血压联盟主席: 高血压诊断标准下调不适合我国国情[N/OL]. 第一财经日报. 第A04版. (2022-11-16). https://www.yicai.com/news/101595160.html. |
| QIAN T X. Chairman of the Chinese Hypertension Alliance: Downregulation of hypertension diagnostic criteria is not suitable for China's national conditions[N/OL]. China Business News. A04. (2022-11-16). https://www.yicai.com/news/101595160.html. | |
| [7] |
CUNNINGHAM R L. MECHANISM AND CLINICAL ASPECTS OF CHRONIC ARTERIAL HYPERTENSION[J]. Cal State J Med, 1912, 10(7):303-305.
pmid: 18735632 |
| [8] |
LÜSCHER T F. What is a normal blood pressure?[J]. Eur Heart J, 2018, 39(24):2233-2240.
doi: 10.1093/eurheartj/ehy330 pmid: 29893817 |
| [9] |
KOTCHEN T A. Historical trends and milestones in hypertension research: a model of the process of translational research[J]. Hypertension, 2011, 58(4):522-538.
doi: 10.1161/HYPERTENSIONAHA.111.177766 pmid: 21859967 |
| [10] |
MOSER M, ROCCELLA E J. The treatment of hypertension: a remarkable success story[J]. J Clin Hypertens (Greenwich), 2013, 15(2):88-91.
doi: 10.1111/jch.12033 pmid: 23339725 |
| [11] |
Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. A cooperative study[J]. JAMA, 1977, 237(3):255-261.
doi: 10.1001/jama.1977.03270300059008 URL |
| [12] |
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The 1980 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure[J]. Arch Intern Med, 1980, 140(10):1280-1285.
pmid: 6775608 |
| [13] |
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The 1984 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure[J]. Arch Intern Med, 1984, 144(5):1045-1057.
pmid: 6143542 |
| [14] |
1988 Joint National Committee. The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure[J]. Arch Intern Med, 1988, 148(5):1023-1038.
pmid: 3365073 |
| [15] |
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure JNC V[J]. Arch Intern Med, 1993, 153(2):154-183.
doi: 10.1001/archinte.1993.00410020010002 URL |
| [16] |
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure[J]. Arch Intern Med, 1997, 157(21):2413-2446.
doi: 10.1001/archinte.157.21.2413 pmid: 9385294 |
| [17] |
CHOBANIAN A V, BAKRIS G L, BLACK H R, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report[J]. JAMA, 2003, 289(19):2560-2572.
doi: 10.1001/jama.289.19.2560 URL |
| [18] | BÜHLER F R, DOYLE A E, EPSTEIN F H, et al. Guidelines for the treatment of mild hypertension: memorandum from a WHO/ISH meeting[J]. Bull World Health Organ, 1983, 61(1):53-56. |
| [19] |
ZANCHETTI A, CHALMERS J P, ARAKAWA K, et al. The 1993 guidelines for the management of mild hypertension: memorandum from a WHO/ISH meeting[J]. Blood Press, 1993, 2(2):86-100.
doi: 10.3109/08037059309077535 URL |
| [20] | 刘力生, 龚兰生. 中国高血压防治指南(试行本)[J]. 中国医药导刊, 2000, 2(1):3-25. |
| LIU L S, GONG L S. Chinese Guidelines for the Prevention and Treatment of Hypertension (Trial Version)[J]. Chin J Med Guide, 2000, 2(1):3-25. | |
| [21] |
European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension[J]. J Hypertens, 2003, 21(6):1011-1053.
doi: 10.1097/00004872-200306000-00001 pmid: 12777938 |
| [22] |
WILLIAMS B, MANCIA G, SPIERING W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension[J]. Eur Heart J, 2018, 39(33):3021-3104.
doi: 10.1093/eurheartj/ehy339 pmid: 30165516 |
| [23] |
WILLIAMS B, POULTER N R, BROWN M J, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV[J]. J Hum Hypertens, 2004, 18(3):139-185.
doi: 10.1038/sj.jhh.1001683 pmid: 14973512 |
| [24] | National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management[EB/OL]. NICE guideline (NG 136).(2022-3-18) [2023-7-11]. https://www.nice.org.uk/guidance/ng136. |
| [25] |
EVANS J G, ROSE G. Hypertension[J]. Br Med Bull, 1971, 27(1):37-42.
doi: 10.1093/oxfordjournals.bmb.a070812 URL |
| [26] |
LEWINGTON S, CLARKE R, QIZILBASH N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies[J]. Lancet, 2002, 360(9349):1903-1913.
doi: 10.1016/s0140-6736(02)11911-8 pmid: 12493255 |
| [27] |
LIU L, ZHANG Y, LIU G, et al. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients[J]. J Hypertens, 2005, 23(12):2157-2172.
doi: 10.1097/01.hjh.0000194120.42722.ac pmid: 16269957 |
| [28] |
THOMOPOULOS C, PARATI G, ZANCHETTI A. Effects at different baseline and achieved blood pressure levels--overview and meta-analyses of randomized trials[J]. J Hypertens, 2014, 32(12):2296-2304.
doi: 10.1097/HJH.0000000000000379 URL |
| [29] |
BRUNSTRÖM M, CARLBERG B. Association of Blood Pressure Lowering With Mortality and Cardiovascular Disease Across Blood Pressure Levels: A Systematic Review and Meta-analysis[J]. JAMA Intern Med, 2018, 178(1):28-36.
doi: 10.1001/jamainternmed.2017.6015 pmid: 29131895 |
| [30] | National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management[C/OL]. Evidence review for initiating treatment. NICE guideline (NG 136).(2019-8) [2023-7-11]. https://www.nice.org.uk/guidance/ng136/evidence/c-initiating-treatment-pdf-6896748208. |
| [31] |
PATER C. The Blood Pressure "Uncertainty Range"-a pragmatic approach to overcome current diagnostic uncertainties (II)[J]. Curr Control Trials Cardiovasc Med, 2005, 6(1):5.
doi: 10.1186/1468-6708-6-5 URL |
| [32] |
ZANCHETTI A, GRASSI G, MANCIA G. When should antihypertensive drug treatment be initiated and to what levels should systolic blood pressure be lowered? A critical reappraisal[J]. J Hypertens, 2009, 27(5):923-934.
doi: 10.1097/HJH.0b013e32832aa6b5 pmid: 19381107 |
| [33] |
MANCIA G, LAURENT S, AGABITI-ROSEI E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document[J]. J Hypertens, 2009, 27(11):2121-2158.
doi: 10.1097/HJH.0b013e328333146d pmid: 19838131 |
| [34] |
BÖHM M, SCHUMACHER H, TEO K K, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials[J]. Lancet, 2017, 389(10085):2226-2237.
doi: S0140-6736(17)30754-7 pmid: 28390695 |
| [35] |
MANCIA G, KJELDSEN S E, ZAPPE D H, et al. Cardiovascular outcomes at different on-treatment blood pressures in the hypertensive patients of the VALUE trial[J]. Eur Heart J, 2016, 37(12):955-964.
doi: 10.1093/eurheartj/ehv633 pmid: 26590384 |
| [36] |
VERDECCHIA P, STAESSEN J A, ANGELI F, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial[J]. Lancet, 2009, 374(9689):525-533.
doi: 10.1016/S0140-6736(09)61340-4 pmid: 19683638 |
| [37] |
CARLBERG B. Time to lower treatment BP targets for hypertension?[J]. Lancet, 2009, 374(9689):503-504.
doi: 10.1016/S0140-6736(09)61467-7 pmid: 19683626 |
| [38] |
CHOBANIAN A V, BAKRIS G L, BLACK H R, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure[J]. Hypertension, 2003, 42(6):1206-1252.
doi: 10.1161/01.HYP.0000107251.49515.c2 pmid: 14656957 |
| [39] |
WRIGHT JT JR, BAKRIS G, GREENE T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial[J]. JAMA, 2002, 288(19):2421-2431.
doi: 10.1001/jama.288.19.2421 URL |
| [40] |
MANCIA G, DE BACKER G, DOMINICZAK A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2007, 28(12):1462-1536.
doi: 10.1093/eurheartj/ehm236 pmid: 17562668 |
| [41] | 中国高血压防治指南修订委员会. 中国高血压防治指南2010[J]. 中华心血管病杂志, 39(7):579-616. |
| LIU L S, Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension[J]. Zhonghua Xin Xue Guan Bing Za Zhi, 39(7):579-615. | |
| [42] |
SCHRIER R W, ESTACIO R O, ESLER A, et al. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes[J]. Kidney Int, 2002, 61(3):1086-1097.
doi: 10.1046/j.1523-1755.2002.00213.x pmid: 11849464 |
| [43] | WEBER M A, MATERSON B J. Hypertension guidelines: a major reappraisal critically examines the available evidence[J]. J Clin Hypertens(Greenwich), 2010, 12(4):229-236. |
| [44] |
ARONOW W S. What should the optimal blood pressure goal be in patients with diabetes mellitus or chronic kidney disease?[J]. Arch Med Sci, 2012, 8(3):399-402.
doi: 10.5114/aoms.2012.29395 pmid: 22851990 |
| [45] | 施仲伟. 血压目标将有回调,综合干预必须加强:从指南更新看高血压防治新动向[J]. 中华高血压杂志, 2012, 20(6):512-514. |
| SHI Z W. The blood pressure target will have a correction, and comprehensive intervention must be strengthened: new trends in hypertension prevention and control seen from the update of guidelines[J]. Chin J Hypertens, 2012, 20(6):512-514. | |
| [46] |
MANCIA G, FAGARD R, NARKIEWICZ K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2013, 34(28):2159-2219.
doi: 10.1093/eurheartj/eht151 pmid: 23771844 |
| [47] |
American Diabetes Association. Standards of medical care in diabetes—2013[J]. Diabetes Care, 2013, 36(Suppl 1):S11-S66.
doi: 10.2337/dc13-S011 URL |
| [48] | WHELTON P K, CAREY R M, ARONOW W S, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines[J]. Hypertension, 2018, 71(6):e13-e115. |
| [49] |
UMEMURA S, ARIMA H, ARIMA S, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019)[J]. Hypertens Res, 2019, 42(9):1235-1481.
doi: 10.1038/s41440-019-0284-9 pmid: 31375757 |
| [50] |
RABI D M, MCBRIEN K A, SAPIR-PICHHADZE R, et al. Hypertension Canada's 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children[J]. Can J Cardiol,2020, 36(5):596-624.
doi: 10.1016/j.cjca.2020.02.086 URL |
| [51] |
WILMOT K A, O'FLAHERTY M, CAPEWELL S, et al. Coronary Heart Disease Mortality Declines in the United States From 1979 Through 2011: Evidence for Stagnation in Young Adults, Especially Women[J]. Circulation,2015, 132(11):997-1002.
doi: 10.1161/CIRCULATIONAHA.115.015293 URL |
| [52] |
MA J, WARD E M, SIEGEL R L, et al. Temporal Trends in Mortality in the United States, 1969-2013[J]. JAMA, 2015, 314(16):1731-1739.
doi: 10.1001/jama.2015.12319 pmid: 26505597 |
| [53] |
SIDNEY S, QUESENBERRY CP JR, JAFFE M G, et al. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals[J]. JAMA Cardiol, 2016, 1(5):594-599.
doi: 10.1001/jamacardio.2016.1326 pmid: 27438477 |
| [54] |
MATERSON B J. JNC 8 at last! No Holy Grail in hand, but useful recommendations[J]. J Clin Hypertens (Greenwich), 2014, 16(4):249-250.
doi: 10.1111/jch.12283 pmid: 24621299 |
| [55] |
FINKS S, REPLEY T L. Sorting it out: what JNC 8 is and what it is not[J]. J Manag Care Spec Pharm, 2015, 21(2):110-112.
doi: 10.18553/jmcp.2015.21.2.110 pmid: 25614999 |
| [56] |
MATERSON B J. JNC 8 transmogrified[J]. J Clin Hypertens (Greenwich), 2013, 15(10):704.
doi: 10.1111/jch.12174 pmid: 24088275 |
| [57] |
BAUCHNER H, FONTANAROSA P B, GOLUB R M. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility[J]. JAMA, 2014, 311(5):477-478.
doi: 10.1001/jama.2013.284432 pmid: 24352759 |
| [58] |
GIBBONS G H, SHURIN S B, MENSAH G A, et al. Refocusing the agenda on cardiovascular guidelines: an announcement from the National Heart, Lung, and Blood Institute[J]. Circulation, 2013, 128(15):1713-1715.
doi: 10.1161/CIRCULATIONAHA.113.004587 pmid: 23785001 |
| [59] |
GIBBONS G H, HAROLD J G, JESSUP M, et al. The next steps in developing clinical practice guidelines for prevention[J]. Circulation, 2013, 128(15):1716-1717.
doi: 10.1161/CIRCULATIONAHA.113.005548 pmid: 23929910 |
| [60] |
JAMES P A, OPARIL S, CARTER B L, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)[J]. JAMA, 2014, 311(5):507-520.
doi: 10.1001/jama.2013.284427 pmid: 24352797 |
| [61] |
BENAVENTE O R, WHITE C L, PEARCE L, et al. The Secondary Prevention of Small Subcortical Strokes (SPS3) study[J]. Int J Stroke, 2011, 6(2):164-175.
doi: 10.1111/j.1747-4949.2010.00573.x pmid: 21371282 |
| [62] |
SPS 3 Investigators; BENAVENTE O R, HART R G, MCCLURE L A, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke[J]. N Engl J Med, 2012, 367(9):817-825.
doi: 10.1056/NEJMoa1204133 URL |
| [63] |
SPS 3 Study Group; BENAVENTE O R, COFFEY C S, CONWIT R, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial[J]. Lancet, 2013, 382(9891):507-515.
doi: 10.1016/S0140-6736(13)60852-1 pmid: 23726159 |
| [64] |
ACCORD Study Group; BUSE J B, BIGGER J T, BYINGTON R P, et al. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods[J]. Am J Cardiol, 2007, 99(12 A):21i-33i.
pmid: 17599422 |
| [65] |
CUSHMAN W C, GRIMM RH JR, CUTLER J A, et al. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial[J]. Am J Cardiol, 2007, 99(12A):44i-55i.
pmid: 17599425 |
| [66] |
ACCORD Study Group; CUSHMAN W C, EVANS G W, BYINGTON R P, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus[J]. N Engl J Med, 2010, 362(17):1575-1585.
doi: 10.1056/NEJMoa1001286 URL |
| [67] | Working Group Report: Expert Panel on a Hypertension Treatment Trial Initiative Meeting Summary[R/OL]. (2007-1-16)[2023-7-8]. https://www.nhlbi.nih.gov/sites/default/files/media/docs/hypertsnsion-full.pdf. |
| [68] |
AMBROSIUS W T, SINK K M, FOY C G, et al. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT)[J]. Clin Trials, 2014, 11(5):532-546.
doi: 10.1177/1740774514537404 pmid: 24902920 |
| [69] |
VERDECCHIA P, ANGELI F, REBOLDI G, et al. The SPRINT trial[J]. J Am Soc Hypertens, 2015, 9(10):750-753.
doi: S1933-1711(15)00667-1 pmid: 26506129 |
| [70] |
SPRINT Research Group; WRIGHT JT JR, WILLIAMSON J D, WHELTON P K, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control[J]. N Engl J Med, 2015, 373(22):2103-2116.
doi: 10.1056/NEJMoa1511939 URL |
| [71] |
GREENLAND P, PETERSON E. The New 2017 ACC/AHA Guidelines “Up the Pressure” on Diagnosis and Treatment of Hypertension[J]. JAMA, 2017, 318(21):2083-2084.
doi: 10.1001/jama.2017.18605 URL |
| [72] |
Kidney Disease: Improving Global Outcomes KDIGO Blood Pressure Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease[J]. Kidney Int, 2021, 99(3S):S1-S87.
doi: 10.1016/j.kint.2020.11.003 URL |
| [73] |
MYERS M G, GODWIN M, DAWES M, et al. Measurement of blood pressure in the office: recognizing the problem and proposing the solution[J]. Hypertension, 2010, 55(2):195-200.
doi: 10.1161/HYPERTENSIONAHA.109.141879 pmid: 20038756 |
| [74] |
KJELDSEN S E, LUND-JOHANSEN P, NILSSON P M, et al. Unattended Blood Pressure Measurements in the Systolic Blood Pressure Intervention Trial: Implications for Entry and Achieved Blood Pressure Values Compared With Other Trials[J]. Hypertension, 2016, 67(5):808-812.
doi: 10.1161/HYPERTENSIONAHA.116.07257 pmid: 27001295 |
| [75] |
BUNDY J D, LI C, STUCHLIK P, et al. Systolic Blood Pressure Reduction and Risk of Cardiovascular Disease and Mortality: A Systematic Review and Network Meta-analysis[J]. JAMA Cardiol, 2017, 2(7):775-781.
doi: 10.1001/jamacardio.2017.1421 pmid: 28564682 |
| [76] |
BAKRIS G L. The Implications of Blood Pressure Measurement Methods on Treatment Targets for Blood Pressure[J]. Circulation, 2016, 134(13):904-905.
doi: 10.1161/CIRCULATIONAHA.116.022536 pmid: 27576778 |
| [77] | BAKRIS G L. Response by Bakris to Letter Regarding Article, "The Implications of Blood Pressure Measurement Methods on Treatment Targets for Blood Pressure"[J]. Circulation, 2017, 135(7):e47. |
| [78] |
WILLIAMSON J D, SUPIANO M A, APPLEGATE W B, et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged ≥75 Years: A Randomized Clinical Trial[J]. JAMA, 2016, 315(24):2673-2682.
doi: 10.1001/jama.2016.7050 pmid: 27195814 |
| [79] |
JOHNSON K C, WHELTON P K, CUSHMAN W C, et al. Blood Pressure Measurement in SPRINT (Systolic Blood Pressure Intervention Trial)[J]. Hypertension, 2018, 71(5):848-857.
doi: 10.1161/HYPERTENSIONAHA.117.10479 pmid: 29531173 |
| [80] |
FILIPOVSKÝ J, SEIDLEROVÁ J, KRATOCHVÍL Z, et al. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients[J]. Blood Press, 2016, 25(4):228-234.
doi: 10.3109/08037051.2015.1134086 URL |
| [81] |
AGARWAL R. Implications of Blood Pressure Measurement Technique for Implementation of Systolic Blood Pressure Intervention Trial (SPRINT)[J]. J Am Heart Assoc, 2017, 6(2):e004536.
doi: 10.1161/JAHA.116.004536 URL |
| [82] |
BAUER F, SEIBERT F S, ROHN B, et al. Attended Versus Unattended Blood Pressure Measurement in a Real Life Setting[J]. Hypertension, 2018, 71(2):243-249.
doi: 10.1161/HYPERTENSIONAHA.117.10026 pmid: 29255074 |
| [83] |
PAINI A, BERTACCHINI F, STASSALDI D, et al. Unattended versus attended blood pressure measurement: Mean values and determinants of the difference[J]. Int J Cardiol, 2019, 274:305-310.
doi: S0167-5273(18)30951-3 pmid: 29945805 |
| [84] |
CHENG R Z, BHALLA V, CHANG T I, et al. Comparison of routine and automated office blood pressure measurement[J]. Blood Press Monit, 2019, 24(4):174-178.
doi: 10.1097/MBP.0000000000000392 pmid: 31116155 |
| [85] |
YUSUF S, LONN E. The SPRINT and the HOPE-3 Trial in the Context of Other Blood Pressure-Lowering Trials[J]. JAMA Cardiol, 2016, 1(8):857-858.
doi: 10.1001/jamacardio.2016.2169 pmid: 27602555 |
| [86] |
FILIPPONE E J, FOY A J. Blood pressure management in the wake of SPRINT[J]. Clev Clin J Med, 2016, 83(3):196-198.
doi: 10.3949/ccjm.83a.16015 pmid: 26974990 |
| [87] |
KJELDSEN S E, NARKIEWICZ K, HEDNER T, et al. The SPRINT study: Outcome may be driven by difference in diuretic treatment demasking heart failure and study design may support systolic blood pressure target below 140 mmHg rather than below 120 mmHg[J]. Blood Press, 2016, 25(2):63-66. 88.
doi: 10.3109/08037051.2015.1130775 URL |
| [88] |
LONN E M, YUSUF S. Should Patients With Cardiovascular Risk Factors Receive Intensive Treatment of Hypertension to <120/80 mm Hg Target? An Antagonist View From the HOPE-3 Trial (Heart Outcomes Evaluation-3)[J]. Circulation, 2016, 134(18):1311-1313.
doi: 10.1161/CIRCULATIONAHA.116.023264 URL |
| [89] |
SHAPIRO B P, AMBROSIUS W T, BLACKSHEAR J L, et al. Impact of Intensive Versus Standard Blood Pressure Management by Tertiles of Blood Pressure in SPRINT (Systolic Blood Pressure Intervention Trial)[J]. Hypertension, 2018, 71:1064-1074.
doi: 10.1161/HYPERTENSIONAHA.117.10646 pmid: 29712745 |
| [90] | LONN E, BOSCH J, POGUE J, et al. Novel Approaches in Primary Cardiovascular Disease Prevention: The HOPE-3 Trial Rationale, Design, and Participants' Baseline Characteristics[J]. Can J Cardiol, 2016, 36(3):311-318. |
| [91] |
LONN E M, BOSCH J, LÓPEZ-JARAMILLO P, et al. Blood-Pressure Lowering in Intermediate-Risk Persons without Cardiovascular Disease[J]. N Engl J Med, 2016, 374(21):2009-2020.
doi: 10.1056/NEJMoa1600175 URL |
| [92] |
PAIS P, JUNG H, DANS A, et al. Impact of blood pressure lowering, cholesterol lowering and their combination in Asians and non-Asians in those without cardiovascular disease: an analysis of the HOPE 3 study[J]. Eur J Prev Cardiol, 2019, 26(7):681-697.
doi: 10.1177/2047487318819019 pmid: 30537846 |
| [93] |
ZHANG S, WU S, REN J, et al. Strategy of blood pressure intervention in the elderly hypertensive patients (STEP): Rational, design, and baseline characteristics for the main trial[J]. Contemp Clin Trials, 2020, 89:105913.
doi: 10.1016/j.cct.2019.105913 URL |
| [94] | 张宇清, 苗欢欢, 杨世杰, 等. 谋定后动——新近高血压重要研究中的启示[J]. 中国介入心脏病学杂志, 2022, 30(7):518-521. |
| ZHANG Y Q, MIAO H H, YANG S J, et al. Planning after Action: Enlightenment from Recent Important Research on Hypertension[J]. Chin J Interv Cardiol, 2022, 30(7):518-521. | |
| [95] |
ZHANG W, ZHANG S, DENG Y, et al. Trial of Intensive Blood-Pressure Control in Older Patients with Hypertension[J]. N Engl J Med, 2021, 385(14):1268-1279.
doi: 10.1056/NEJMoa2111437 URL |
| [96] |
NELSON M R. Moving the Goalposts for Blood Pressure-Time to Act[J]. N Engl J Med, 2021, 385(14):1328-1329.
doi: 10.1056/NEJMe2112992 URL |
| [97] |
BENETOS A, PERSU A, KREUTZ R. Hypertension in older patients: a STEP forward?[Formula: see text][J]. Blood Press, 2022, 31(1):118-120.
doi: 10.1080/08037051.2022.2075826 URL |
| [98] |
UNGER T, BORGHI C, CHARCHAR F, et al. 2020 International Society of Hypertension global hypertension practice guidelines[J]. J Hypertens, 2020, 38(6):982-1004.
doi: 10.1097/HJH.0000000000002453 pmid: 32371787 |
| [99] |
AL-MAKKI A, DIPETTE D, WHELTON P K, et al. Hypertension Pharmacological Treatment in Adults: A World Health Organization Guideline Executive Summary[J]. Hypertension, 2022, 79(1):293-301.
doi: 10.1161/HYPERTENSIONAHA.121.18192 URL |
| [100] |
MANCIA G, KREUTZ R, BRUNSTRÖM M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA)[J]. J Hypertens, 2023, 41(12):1874-2071.
doi: 10.1097/HJH.0000000000003480 URL |
| [101] |
CHEN X, BARYWANI S B, HANSSON P O, et al. High-normal blood pressure conferred higher risk of cardiovascular disease in a random population sample of 50-year-old men: A 21-year follow-up[J]. Medicine (Baltimore), 2020, 99(17):e19895.
doi: 10.1097/MD.0000000000019895 URL |
| [102] |
MUSCAT D M, MORRIS G M, BELL K, et al. Benefits and Harms of Hypertension and High-Normal Labels: A Randomized Experiment[J]. Circ Cardiovasc Qual Outcomes, 2021, 14(4):e007160.
doi: 10.1161/CIRCOUTCOMES.120.007160 URL |
| [103] |
HAMER M, BATTY G D, STAMATAKIS E, et al. Hypertension awareness and psychological distress[J]. Hypertension, 2010, 56(3):547-550.
doi: 10.1161/HYPERTENSIONAHA.110.153775 pmid: 20625078 |
| [104] |
RANTANEN A T, KORKEILA J J A, LÖYTTYNIEMI E S, et al. Awareness of hypertension and depressive symptoms: a cross-sectional study in a primary care population[J]. Scand J Prim Health Care, 2018, 36(3):323-328.
doi: 10.1080/02813432.2018.1499588 URL |
| [105] | 王继光. 必须高度重视降压药物治疗的安全性[J]. 中华心血管病杂志, 2022, 50(7):625-626. |
| WANG J G. [Taking the safety of antihypertensive drug treatment seriously][J]. Zhonghua Xin Xue Guan Bing Za Zhi, 2022, 50(7):625-626. | |
| [106] | 潘锋. CHINOM研究填补国内外心血管疾病同类研究空白——正常高值血压人群如无其他严重疾病无需服用降压药[J]. 中国医药科学, 2022, 12(11):1-4. |
| PAN F. CHINOM research fills the gap in similar research on cardiovascular diseases both domestically and internationally - people with normal high blood pressure do not need to take antihypertensive drugs if there are no other serious diseases[J]. China Med Pharm, 2022, 12(11):1-4. | |
| [107] | 医师报循环频道. 该怎么看待CHINOM研究?张新华教授等独家解读[EB/OL]. 医师报循环频道.(2022-5-17) [2023-7-17]. https://mp.pdnews.cn/Pc/ArtInfoApi/article?id=28689628. |
| [108] |
KREUTZ R, BRUNSTRÖM M, THOMOPOULOS C, et al. Do recent meta-analyses truly prove that treatment with blood pressure-lowering drugs is beneficial at any blood pressure value, no matter how low? A critical review[J]. J Hypertens, 2022, 40(5):839-846.
doi: 10.1097/HJH.0000000000003056 URL |
| [109] |
BASSLER D, MONTORI V M, BRIEL M, et al. Early stopping of randomized clinical trials for overt efficacy is problematic[J]. J Clin Epidemiol, 2008, 61(3):241-246.
doi: 10.1016/j.jclinepi.2007.07.016 pmid: 18226746 |
| [110] |
NOLDE J M, BEANEY T, CARNAGARIN R, et al. Global Impact of Different Blood Pressure Thresholds in 4 021 690 Participants of the May Measurement Month Initiative[J]. Hypertension, 2022, 79(7):1497-1505.
doi: 10.1161/HYPERTENSIONAHA.122.19144 URL |
| [1] | 钱莹, 马晓波, 高琛妮, 张春丽, 马骏, 张文, 陈晓农. 慢性肾脏病患者高尿酸血症与高血压的关联分析[J]. 诊断学理论与实践, 2023, 22(02): 160-165. |
| [2] | 杨扬, 吴琴咪, 冯玉兰, 张蓓, 傅毅. 高血压患者脑血管周围间隙扩大和脑腔隙灶相关影响因素[J]. 诊断学理论与实践, 2021, 20(04): 372-377. |
| [3] | 中国高血压联盟《动态血压监测指南》委员会. 2020中国动态血压监测指南[J]. 诊断学理论与实践, 2021, 20(01): 21-36. |
| [4] | 陈歆, 程艾邦, 许建忠, 李燕, 王继光. 中国高血压患者原发性醛固酮增多症的前瞻性筛查研究进展[J]. 诊断学理论与实践, 2020, 19(05): 450-453. |
| [5] | 中国高血压联盟. 高血压患者原发性醛固酮增多症筛查诊治流程[J]. 诊断学理论与实践, 2020, 19(05): 454-459. |
| [6] | 李宙童, 张炜, 王继光. 家庭血压测量诊断白大衣高血压及隐匿性高血压的准确性研究[J]. 诊断学理论与实践, 2020, 19(05): 487-493. |
| [7] | 王春花, 祁爽, 王敏. 原发性醛固酮增多症合并无痛性心肌梗死一例报告[J]. 诊断学理论与实践, 2020, 19(05): 528-530. |
| [8] | 黄永艳, 杨丽娜, 曹久妹, 王巍. 基于云数据的门诊高血压监测[J]. 诊断学理论与实践, 2020, 19(03): 319-324. |
| [9] | 王亚娟, 郭芊卉, 张冬燕, 程艾邦, 陈凌, 朱鼎良, 李燕. 上海莘庄社区儿童及青少年超重、肥胖的发生率及血压相关因素分析[J]. 诊断学理论与实践, 2019, 18(05): 575-580. |
| [10] | 施仲伟. SPRINT试验诚信不足无力改变高血压治疗目标值[J]. 诊断学理论与实践, 2017, 16(06): 576-581. |
| [11] | 蒋雄京, 董徽. 经导管射频消融去肾神经治疗高血压:当前问题与展望[J]. 诊断学理论与实践, 2017, 16(06): 567-570. |
| [12] | 陈卉, 郭芊卉, 许杰, 程艾邦, 张冬燕, 王颖, 黄绮芳, 盛长生, 李燕. 经颅多普勒超声研究无症状性颅内动脉狭窄的患病情况及影响因素[J]. 诊断学理论与实践, 2017, 16(06): 592-595. |
| [13] | 李燕, 张冬燕. 重视隐匿性高血压的筛查诊断与治疗[J]. 诊断学理论与实践, 2017, 16(06): 571-575. |
| [14] | 慕瑾瑾, 杨康, 冯玉兰, 傅毅. 高血压性脑出血患者伴新发无症状性脑梗死的相关危险因素分析及预后的探讨[J]. 诊断学理论与实践, 2016, 15(05): 492-497. |
| [15] | 谷晓岚, 魏雪, 牛敏, 罗兰, 李欣宇, 高政南,. 大连地区中老年人群中颈围与高血压的相关性研究[J]. 诊断学理论与实践, 2016, 15(04): 371-375. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
