

Journal of Diagnostics Concepts & Practice ›› 2024, Vol. 23 ›› Issue (04): 405-415.doi: 10.16150/j.1671-2870.2024.04.009
• Original articles • Previous Articles Next Articles
GU Tianyan1,3, PAN Jingyu2, CHEN Lin3, ZOU Zhihao4, SHI Qinghai3( )
)
Received:2024-01-02
Accepted:2024-06-03
Online:2024-08-25
Published:2024-08-25
Contact:
SHI Qinghai
E-mail:shiqinghai@aliyun.com
CLC Number:
GU Tianyan, PAN Jingyu, CHEN Lin, ZOU Zhihao, SHI Qinghai. The value of inflammatory cytokines(TNF-α, IL-6 and IL-8) in predicting prognosis in patients with new-onset intracerebral hemorrhage[J]. Journal of Diagnostics Concepts & Practice, 2024, 23(04): 405-415.
Table 1
Comparison of baseline information between study and control groups
| Characteristic | ICH group (n=40) | Control group (n=40) | t/χ2 value | P value |
|---|---|---|---|---|
| Age (years) | 59.10±12.84 | 58.93±12.52 | 0.051 | 0.960 |
| Sex [n (%)] | 0.054 | 0.816 | ||
| Male | 26(65) | 25(62.5) | ||
| Female | 14(35) | 15(37.5) | ||
| Hypertensive [n (%)] | 18(45) | 13(32.5) | 1.317 | 0.251 |
| Diabetes [n (%)] | 6(15) | 8(20) | 0.346 | 0.556 |
| Cardiology [n (%)] | 3(7.5) | 5(12.5) | 0.556 | 0.456 |
| BMI (kg/m2) | 23.49±4.16 | 22.22±3.42 | 1.550 | 0.125 |

Figure 1
Differences in the serum expression levels of TNF-α, IL-6 and IL-8 between the study and control groups The expression levels of (A) TNF-α (P<0.000 1); (B) IL-6 (P<0.000 1); and (C) IL-8 (P<0.000 1) were elevated in the study group. Note: All data are expressed as M (P25, P75), ****P<0.000 1. Abbreviations: CTL, control, n=40; ICH, intracerebral hemorrhage, n=40. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
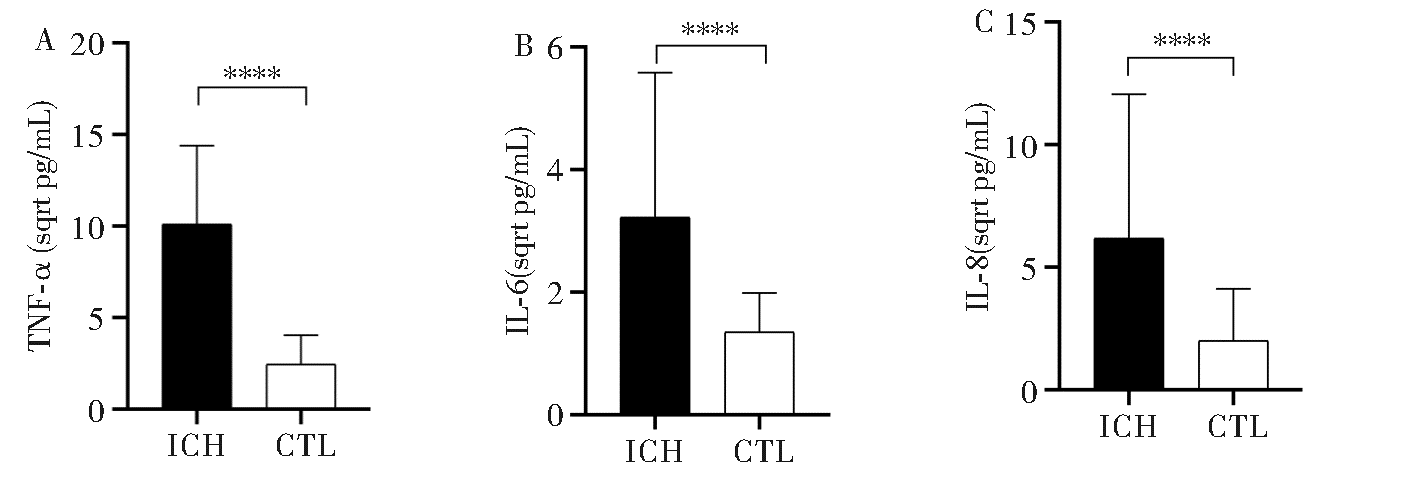

Figure 2
Differences in the expression levels of TNF-α, IL-6, and IL-8 in the cerebrospinal fluid between the study and control groups The expression levels of (A) TNF-α (P<0.000 1); (B) IL-6 (P<0.000 1); and (C) IL-8 (P<0.000 1) were elevated in the study group. Note: All data are expressed as M (P25, P75), ****P<0.000 1. Abbreviations: CTL, control, n=40; ICH, intracerebral hemorrhage, n=40. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
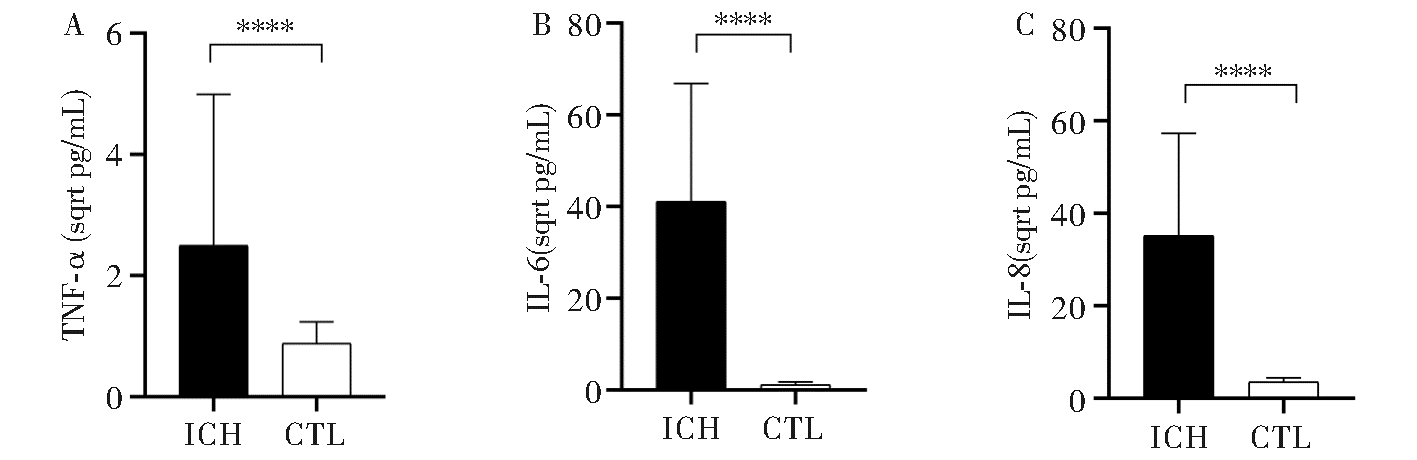

Figure 3
Differences in serum TNF-α, IL-6 and IL-8 expression levels in intracerebral hemorrhage patients with different GCS scores (A) The serum levels of TNF-α in intracerebral hemorrhage patients with a GCS score of 3-8 were higher than those with a GCS score of 9-15 (P<0.01), (B) The serum levels of IL-6 in intracerebral hemorrhage patients with a GCS score of 3-8 were significantly higher than those with a GCS score of 9-15 (P<0.01), (C) The serum levels of IL-8 in intracerebral hemorrhage patients with a GCS score of 3-8 were significantly higher than those with a GCS score of 9-15 points (P<0.01). Note: All data are expressed as M (P25, P75), **: P < 0.01. GCS was 3 to 8 points, n=26; GCS was 9 to 15 points, n=14. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
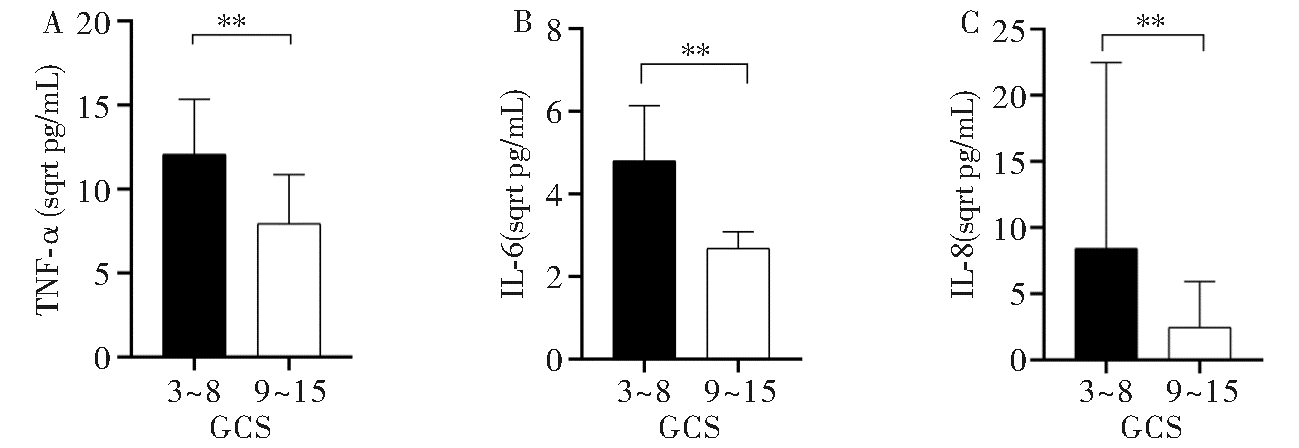

Figure 4
Differences in TNF-α, IL-6 and IL-8 expression levels in cerebrospinal fluid of intracerebral hemorrhage patients with different GCS (A) TNF-α levels in the cerebrospinal fluid of patients with intracerebral hemorrhage with GCS of 3-8 were higher than those with GCS of 9-15 (P<0.001), (B) IL-6 levels in the cerebrospinal fluid of patients with intracerebral hemorrhage with GCS of 3-8 were significantly higher than those with GCS of 9-15 (P<0.001), (C) IL-8 levels in the cerebrospinal fluid of patients with intracerebral hemorrhage with GCS of 3-8 were significantly higher than those with GCS of 9-15 points (P<0. 01). Note: All data are expressed as M (P25, P75), ***: P<0.001,**: P<0.01. GCS was 3 to 8 points, n=26; GCS was 9 to 15 points, n=14. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
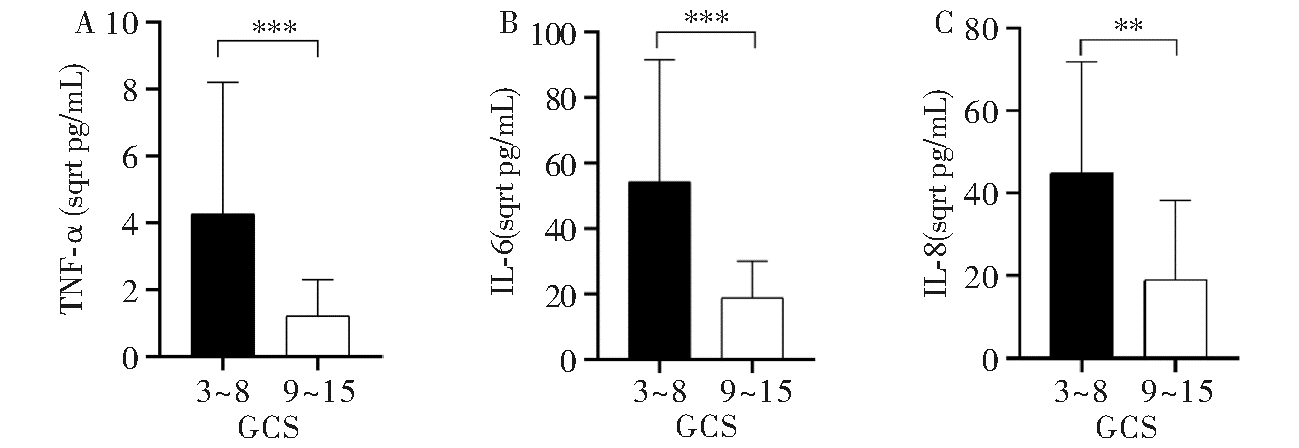

Figure 5
Expression levels of TNF-α, IL-6 and IL-8 in serum of patients with intracerebral hemorrhage of different blee-ding volume (A) The difference of serum TNF-α level was not statistically significant between the bleeding volume ≥30 mL group and the bleeding volume <30 mL group (P>0.05), (B) The serum IL-6 level of patients in the bleeding volume ≥30 mL group was higher than that of the bleeding volume <30 mL group (P<0.05), and (C) The serum IL-8 level of the patients in the bleeding volume ≥30 mL group and the bleeding volume <30 mL group The difference was not statistically significant (P>0.05). Note: All data are expressed as M (P25, P75), *: P<0.05, ns P>0.05. The bleeding volume ≥30 mL group, n=21; the bleeding volume <30 mL group, n=19. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
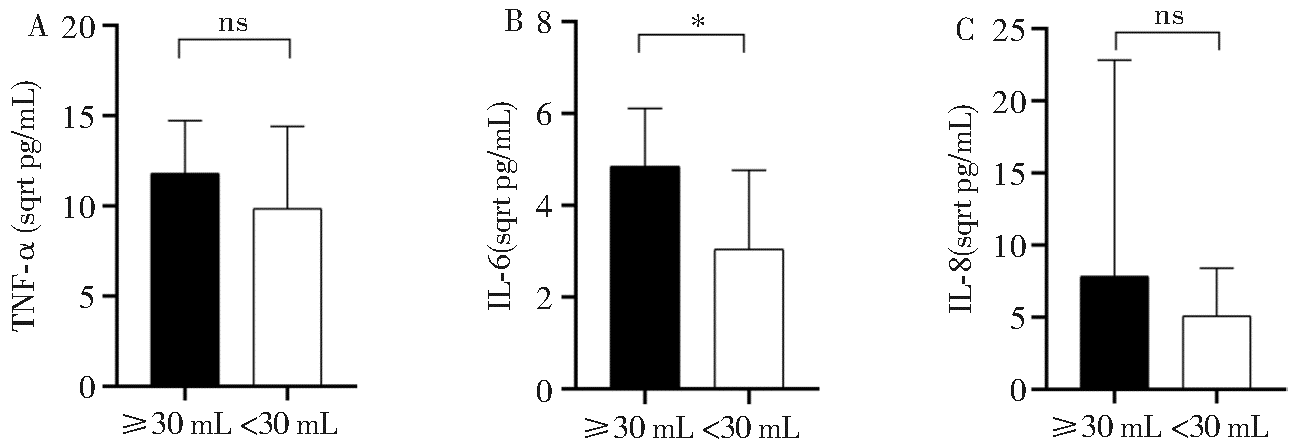

Figure 6
Expression levels of TNF-α, IL-6 and IL-8 in the cerebrospinal fluid of patients with intracerebral hemorrhage of different bleeding volumes (A) TNF-α level in cerebrospinal fluid of patients in the bleeding volume ≥30 mL group was higher than that in the bleeding volume <30 mL group (P<0.05), (B) IL-6 level in cerebrospinal fluid of patients in the bleeding volume ≥30 mL group was higher than that in the bleeding volume <30 mL group (P<0.001), (C) IL-8 level in cerebrospinal fluid of patients in the bleeding volume ≥30 mL group was higher than that in the bleeding volume <30 mL group (P< 0.05). Note: All data are expressed as M (P25, P75), ***: P<0.001,*: P<0.05. The bleeding volume ≥30mL group, n=21; the bleeding volume <30 mL group, n=19. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
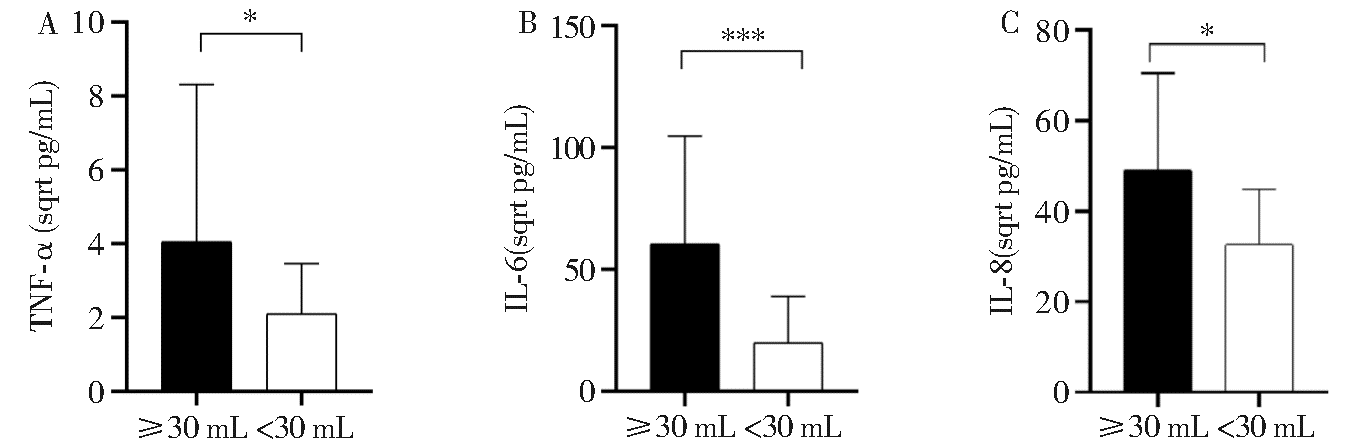
Table 2
Comparison of indicators in the good prognosis group and the poor prognosis group
| Characteristic | Favorable(n=18) | Unfavorable(n=22) | t/χ2/Z value | P value |
|---|---|---|---|---|
| Age (years) | 56.39±14.37 | 61.91±12.04 | 1.323 | 0.194 |
| Sex [n (%)] | 0.559 | 0.455 | ||
| Male | 12 (66.7) | 17 (77.3) | ||
| Female | 6 (33.3) | 5 (22.7) | ||
| Hypertensive [n (%)] | 5 (27.8) | 13 (59.1) | 3.922 | <0.05 |
| Diabetes [n (%)] | 2 (11.1) | 4 (18.2) | 0.388 | 0.533 |
| Cardiology [n (%)] | 2 (7.1) | 1 (12.5) | 0.615 | 0.433 |
| Hematoma location [n (%)] | 1.397 | 0.806 | ||
| Basal ganglia | 8 (44.4) | 11 (50) | ||
| Thalamus | 3 (16.7) | 5 (22.7) | ||
| Lobar | 4 (22.2) | 2 (9.1) | ||
| Other | 3 (16.7) | 4 (18.2) | ||
| GCS (points) | 10.56±3.49 | 5.68±2.06 | -5.502 | <0.000 1 |
| ICH volume(mL) [n (%)] | 4.821 | <0.05 | ||
| ≥30 mL | 6 (33.3) | 15 (68.2) | ||
| <30 mL | 12 (66.7) | 7 (31.8) | ||
| Blood sugar (mmol/L) | 6.57 (5.58, 7.13) | 10.16 (7.78, 12.90) | -3.833 | <0.000 1 |
| Albumin (g/L) | 39.28±3.77 | 36.96±4.03 | -1.866 | 0.070 |
| Calcitonin (ng/mL) | 0.27 (0.06, 0.57) | 0.10 (0.26, 0.73) | -0.802 | 0.422 |
| WBC (109/L) | 9.92 (7.61, 12.43) | 10.68 (9.01, 12.70) | -0.802 | 0.423 |
| D-dimer (mg/L) | 1.47 (0.36, 2.55) | 1.88 (1.08, 6.03) | -1.495 | 0.135 |

Figure 7
Differences in serum TNF-α, IL-6 and IL-8 expression levels in patients with intracerebral hemorrhage with different GOS (A) The serum levels of TNF-α were significantly higher in patients with a GOS of 1-3 than in patients with a GOS of 4-5 (P<0.01), (B) The serum levels of IL-6 were significantly higher in patients with a GOS of 1-3 than in patients with a GOS of 4-5 (P<0.001), and (C) The serum levels of IL-8 were significantly higher in patients with a GOS of 1-3 than in patients with a GOS of 4-5 (P<0.001). Note: All data are expressed as M (P25, P75), ***: P<0.001,**: P<0.01. GOS was 1-3 points, n=22; GOS was 4-5 points, n=18. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
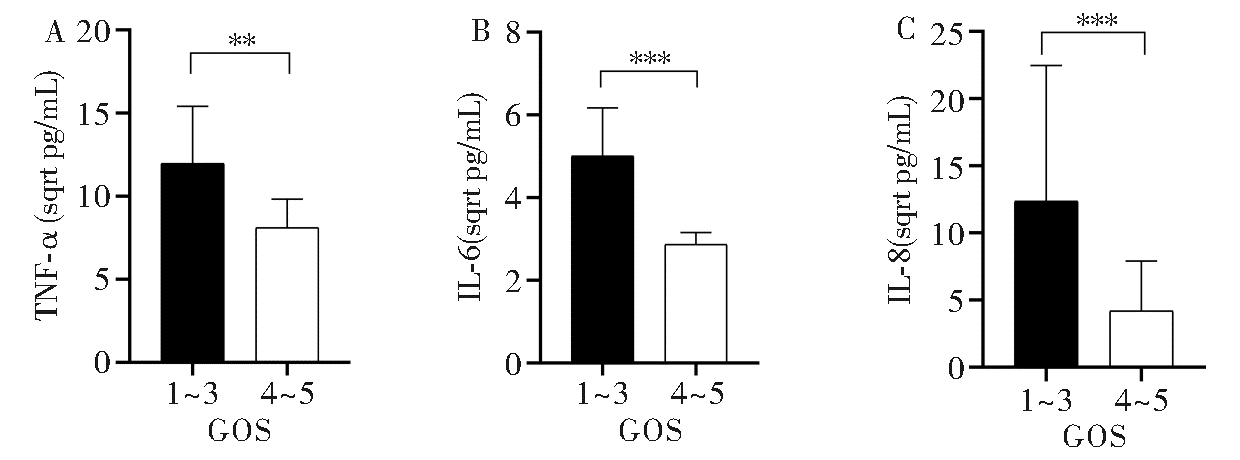

Figure 8
Differences in the expression levels of TNF-α, IL-6 and IL-8 in the cerebrospinal fluid of patients with intracerebral hemorrhage with different GOS (A) TNF-α levels in the cerebrospinal fluid of patients with GOS of 1-3 were significantly higher than those with GOS of 4-5 (P<0.001), (B) IL-6 levels in the cerebrospinal fluid of patients with GOS of 1-3 were significantly higher than those with GOS of 4-5 (P<0.01), and (C) IL-8 levels in the cerebrospinal fluid of patients with GOS of 1-3 were significantly higher than those with GOS of 4-5 (P< 0.001). Note: All data are expressed as M (P25, P75), ***: P<0.001,**: P<0.01. GOS was 1-3 points, n=22; GOS was 4-5 points, n=18. The original result values have been transformed to their square root equivalents to facilitate a more distinct and three-dimensional portrayal of data distribution, denoted in sqrt pg/mL.
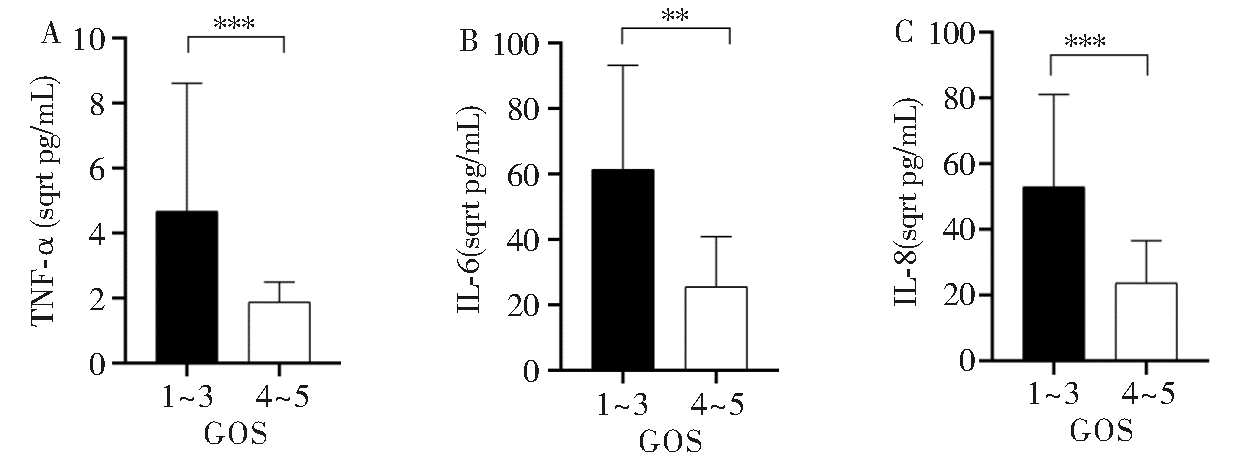
Table 3
Analysis of factors influencing the functional prognosis of patients with intracerebral hemorrhage
| Cytokines | β value | SE | Wald value | OR (95%CI) | P value |
|---|---|---|---|---|---|
| TNF-α in CSF | 0.166 | 0.068 | 6.009 | 1.181 (1.034, 1.349) | 0.014 |
| TNF-α in serum | 0.013 | 0.005 | 6.060 | 1.013 (1.003, 1.023) | 0.014 |
| IL-6 in CSF | 1.702 | 0.845 | 4.054 | 1.000 (1.000, 1.001) | 0.044 |
| IL-6 in serum | 0.093 | 0.034 | 7.230 | 1.097 (1.025, 1.174) | 0.007 |
| IL-8 in CSF | 0.001 | 0.000 | 6.888 | 1.001 (1.000, 1.002) | 0.009 |
| IL-8 in serum | 0.023 | 0.008 | 7.773 | 1.023 (1.007, 1.040) | 0.005 |
| GCS | -0.600 | 0.187 | 10.330 | 0.549 (0.381, 0.791) | 0.001 |
| ICH volume | 1.455 | 0.678 | 4.609 | 4.286 (1.135, 16.18) | 0.032 |
Table 4
Analysis of the prognostic predictive value of serum TNF-α, IL-6, IL-8 levels and the combination for intracerebral hemorrhage
| Cytokines | AUC | Sensitivity (%) | Specificity (%) | 95%CI | Youden index | Cutoff value (pg/mL) | P value |
|---|---|---|---|---|---|---|---|
| TNF-α | 0.692 | 86.4 | 55.6 | 0.524-0.860 | 0.42 | 73.69 | 0.038 8 |
| IL-6 | 0.808 | 77.3 | 88.9 | 0.662-0.953 | 0.662 | 12.79 | 0.000 9 |
| IL-8 | 0.721 | 90.9 | 50.0 | 0.559-0.883 | 0.409 | 13.09 | 0.017 4 |
| Combine | 0.843 | 81.8 | 77.8 | 0.720-0.967 | 0.596 | — | 0.000 2 |
Table 5
Analysis of the prognostic predictive value of cerebrospinal fluid TNF-α, IL-6, IL-8 levels and combination for intracerebral hemorrhage
| Cytokines | AUC | Sensitivity (%) | Specificity (%) | 95%CI | Youden index | Cutoff value (pg/mL) | P value |
|---|---|---|---|---|---|---|---|
| TNF-α | 0.836 | 63.6 | 100 | 0.711-0.961 | 0.636 | 15.60 | 0.000 3 |
| IL-6 | 0.773 | 54.5 | 94.4 | 0.628-0.918 | 0.489 | 3 281.96 | 0.003 3 |
| IL-8 | 0.849 | 68.2 | 94.4 | 0.732-0.965 | 0.626 | 1 982.95 | 0.000 2 |
| Combine | 0.917 | 72.7 | 100 | 0.835-0.999 | 0.727 | — | 0.000 1 |
| [1] | MAGID-BERNSTEIN J, GIRARD R, POLSTER S, et al. Cerebral hemorrhage: pathophysiology, treatment, and future directions[J]. Circ Res, 2022, 130(8):1204-1229. |
| [2] | REN H, HAN R, CHEN X, et al. Potential therapeutic targets for intracerebral hemorrhage-associated inflammation: An update[J]. J Cereb Blood Flow Metab, 2020, 40(9):1752-1768. |
| [3] |
XUE M, YONG V W. Neuroinflammation in intracerebral haemorrhage: immunotherapies with potential for translation[J]. Lancet Neurol, 2020, 19(12):1023-1032.
doi: 10.1016/S1474-4422(20)30364-1 pmid: 33212054 |
| [4] | CHEN S, LI L, PENG C, et al. Targeting oxidative stress and inflammatory response for blood-brain barrier protection in intracerebral hemorrhage[J]. Antioxid Redox Signal, 2022, 37(1-3):115-134. |
| [5] | ZHU H, WANG Z, YU J, et al. Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage[J]. Prog Neurobiol, 2019, 178:101610. |
| [6] | WANG Y, TIAN M, TAN J, et al. Irisin ameliorates neuroinflammation and neuronal apoptosis through integrin αVβ5/AMPK signaling pathway after intracerebral hemorrhage in mice[J]. J Neuroinflammation, 2022, 19(1):82. |
| [7] | HU D, MO X, LUO J, et al. 17-DMAG ameliorates neuroinflammation and BBB disruption via SOX5 mediated PI3K/Akt pathway after intracerebral hemorrhage in rats[J]. Int Immunopharmacol, 2023, 123:110698. |
| [8] | 龚浩, 郑波, 何俊, 等. 急性脑出血病人血清TNF-α、TGF-β1、ICAM-1水平与神经功能损伤及预后的相关性[J]. 中西医结合心脑血管病杂志, 2021, 19(13):2264-2267. |
| GONG H, ZHENG B, HE J, et al. Correlation between serum TNF-α,TGF-β1,ICAM-1 levels and neurological deficit and prognosis in patients with acute intracerebral hemorrhage[J]. Chin J Integr Med Cardio-Cerebrovascular Dis, 2021, 19(13):2264-2267. | |
| [9] | LEASURE A C, KUOHN L R, VANENT K N, et al. Association of serum IL-6 (Interleukin 6) with functional outcome after intracerebral hemorrhage[J]. Stroke, 2021, 52(5):1733-1740. |
| [10] | 刘镇, 韩娟. 血清GFPA、IL-6及MMP9与HICH患者脑出血血肿量、神经功能受损的关系[J]. 国际医药卫生导报, 2019, 25(6):864-867. |
| LIU Z, HAN J. Relationship between serum GFPA, IL-6, and MMP9 and hematoma volume and neurological impairment in patients with HICH[J]. Int Med Health Guid News, 2019, 25(6):864-867. | |
| [11] | 罗乐, 何俊, 刘刚, 等. 脑脊液hs-CRP、IGF-1及IL-6水平与高血压性脑出血神经功能损害程度的相关性[J]. 中国临床神经外科杂志, 2021, 26(1):29-31. |
| LUO L, HE J, LIU G, et al. Correlation of cerebrospinal fluid levels of hs-CRP,IGF-1 and IL-6 with neurological impairment of patients with hypertensive cerebral hemorrhage[J]. Chin J of Clin Neurosurg, 2021, 26(1):29-31. | |
| [12] | 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国脑出血诊治指南(2019)[J]. 中华神经科杂志, 2019, 52(12):994-1005. |
| Chinese Society of Neurology, Chinese Stroke Society. Chinese guidelines for diagnosis and treatment of acute intracerebral hemorrhage 2019[J]. Chin J Neurol, 2019(12): 994-1005. | |
| [13] | MIDDLETON P M. Practical use of the Glasgow Coma Scale; a comprehensive narrative review of GCS methodology[J]. Australas Emerg Nurs J, 2012, 15(3):170-183. |
| [14] |
MCMILLAN T, WILSON L, PONSFORD J, et al. The Glasgow Outcome Scale - 40 years of application and refinement[J]. Nat Rev Neurol, 2016, 12(8):477-485.
doi: 10.1038/nrneurol.2016.89 pmid: 27418377 |
| [15] |
李彩丽, 蒋艳. 脑出血患者血压管理研究现状[J]. 中国现代神经疾病杂志, 2021, 21(2):101-106.
doi: 10.3969/j.issn.1672-6731.2021.02.007 |
| LI C L, JIANG Y. Research status of blood pressure management in cerebral hemorrhage[J]. Chin J Contemp Neurol Neurosurg, 2021, 21(2): 101-106. | |
| [16] |
TU L, LIU X, LI T, et al. Admission serum calcium level as a prognostic marker for intracerebral hemorrhage[J]. Neurocrit Care, 2019, 30(1):81-87.
doi: 10.1007/s12028-018-0574-0 pmid: 29995185 |
| [17] | 陈状, 温锦崇, 江澈, 等. 急性期脑出血患者血清炎症因子IL-6、IL-8及tau蛋白水平的变化的临床潜在价值[J]. 空军医学杂志, 2020, 36(6):489-491,508. |
| CHEN Z, WEN J C, JIANG C, et al. Changes of serum inflammatory factors and tau protein levels in patients with acute intracerebral hemorrhage and their clinical significance[J]. Med J Air Force, 2020, 36(6):489-491,508. | |
| [18] | 左权平. 血清IL-6、 IL-18、 CRP在高血压性脑出血患者中的表达及意义[J]. 中国卫生工程学, 2020, 19(4):578-579. |
| ZUO Q P. The expression and significance of serum IL-6, IL-18, and CRP in patients with hypertensive intracerebral hemorrhage[J]. Chin J Public Health Eng, 2020, 19(4):578-579. | |
| [19] | 李星光, 卢圣奎. ICH损伤中干扰素调节因子4的表达与炎症反应[J]. 脑与神经疾病杂志, 2022, 30(12):766-770. |
| LI X G, LU S K. Expression of interferon regulatory factor 4 and inflammatory in secondary injury of intracerebral hemorrhage[J]. J Brain Nerv Dis, 2022, 30(12):766-770. | |
| [20] | FEJES Z, PÓCSI M, TAKAI J, et al. Preterm intraventricular hemorrhage-induced inflammatory response in human choroid plexus epithelial cells[J]. Int J Mol Sci, 2021, 22(16):8648. |
| [21] | ZIAI W C, PARRY-JONES A R, THOMPSON C B, et al. Early inflammatory cytokine expression in cerebrospinal fluid of patients with spontaneous intraventricular hemorrhage[J]. Biomolecules, 2021, 11(8):1123. |
| [22] | GUSDON A M, THOMPSON C B, QUIRK K, et al. CSF and serum inflammatory response and association with outcomes in spontaneous intracerebral hemorrhage with intraventricular extension: an analysis of the CLEAR-ⅢTrial[J]. J Neuroinflammation, 2021, 18(1):179. |
| [23] |
FAM M D, ZEINEDDINE H A, ELIYAS J K, et al. CSF inflammatory response after intraventricular hemorrhage[J]. Neurology, 2017, 89(15):1553-1560.
doi: 10.1212/WNL.0000000000004493 pmid: 28887375 |
| [24] | 王超, 游潮, 刘窗溪, 等. 高血压脑出血后血浆及脑脊液IL-1β和IL-6在病情评估中的应用价值[J]. 中华神经外科杂志, 2015, 31(11):1158-1160. |
| WANG C, YOU C, LIU C X, et al. Application value of plasma and cerebrospinal fluid IL-1β and IL-6 in disease assessment after hypertensive intracerebral hemorrhage[J]. Chin Neurosurg J, 2015(11): 1158-1160. | |
| [25] | XU Y, MA H Y, QIAO C Y, et al. Significance of changes in the concentration of inflammatory factors in blood or cerebrospinal fluid in evaluating the severity and prognosis of spontaneous cerebral hemorrhage: A systematic review and meta-analysis[J]. Clin Neurol Neurosurg, 2021(205): 106631 |
| [26] | BELARBI K, JOPSON T, TWEEDIE D, et al. TNF-α protein synthesis inhibitor restores neuronal function and reverses cognitive deficits induced by chronic neuroinflammation[J]. J Neuroinflammation, 2012, 9:23. |
| [27] | 张嵘, 何地芹, 李丹青, 等. 自发性脑出血患者血清炎症因子和胶质纤维酸性蛋白水平变化及其临床意义[J]. 中国实用内科杂志, 2023, 43(7):567-572. |
| ZHANG R, HE D Q, LI D Q, et al. Changes and clinical value of serum inflammatory factors and GFAP levels in patients with spontaneous cerebral hemorrhage[J]. Chin J Pract Intern Med, 2023, 43(7):567-572. | |
| [28] |
赵顺忠, 杨彦龙, 杨阳, 等. 自发性小脑出血术后远期预后影响因素分析[J]. 中国现代神经疾病杂志, 2022, 22(10):871-878.
doi: 10.3969/j.issn.1672-6731.2022.10.007 |
| ZHAO S Z, YANG Y L, YANG Y, et al. Analysis of influen-cing factors of long-term prognosis after surgery for spontaneous cerebellar hemorrhage[J]. Chin J Contemp Neurol Neurosurg, 2022, 22(10):871-878. | |
| [29] | 吴佩涛, 杨学, 许州, 等. 颅内压检测及血清HSP70、S100B水平对高血压性脑出血患者预后的预测价值[J]. 新疆医科大学学报, 2022, 45(3):313-317. |
| WU P T, YANG X, XU Z, et al. Predictive value of intracranial pressure and serum HSP70 and S100B levels for prognosis of patients with hypertensive intracerebral hemor-rhage[J]. J Xinjiang Med Univ, 2022, 45(3):313-317. | |
| [30] | 宁书蔚, 柳颖, 赵春刚. GCS-Pupils评分在急性脑出血患者预后评估中的应用效果[J]. 中国医药指南, 2022, 20(26):85-88. |
| NING S W, LIU Y, ZHAO C G. Application effect of GCS scoring on the prognosis evaluation of patient with acute cerebral hemorrhage[J]. Guide Chin Med, 2022, 20(26): 85-88. | |
| [31] | 白玉玲, 刘泓渊. 高血压脑出血患者血清IL-6和TGF-β1水平与脑出血量及神经功能损伤的相关性[J]. 标记免疫分析与临床, 2021, 28(12):2050-2054. |
| BAI Y L, LIU H Y. The correlation between serum IL-6,TGF-β1 levels and cerebral hemorrhage volume,nerve function damage in patients with hypertensive intracerebral hemorrhage[J]. Labeled Immunoassays Clin Med, 2021, 28(12): 2050-2054. | |
| [32] |
LI Q, LAN X, HAN X, et al. Microglia-derived interleukin-10 accelerates post-intracerebral hemorrhage hematoma clearance by regulating CD36[J]. Brain Behav Immun, 2021, 94:437-457.
doi: 10.1016/j.bbi.2021.02.001 pmid: 33588074 |
| [33] | TOBIESON L, GARD A, RUSCHER K, et al. Intracerebral proinflammatory cytokine increase in surgically evacuated intracerebral hemorrhage: A microdialysis study[J]. Neurocrit Care, 2022, 36(3):876-887. |
| [34] | ZHANG X W, WU Y, WANG D K, et al. Expression changes of inflammatory cytokines TNF-α, IL-1β and HO-1 in hematoma surrounding brain areas after intracerebral hemorrhage[J]. J Biol Regul Homeost Agents, 2019, 33(5):1359-1367. |
| [35] | 刘玉敬, 马晴, 梁雅静, 等. 高血压脑出血患者急性期症状群及其与预后生活质量的相关性[J]. 中国临床研究, 2024, 37(2):246-251. |
| LIU Y J, MA Q, LIANG Y J, et al. Symptom clusters in patients with hypertensive cerebral haemorrhage during the acute phase and their correlation with prognostic quality of life[J]. Chin J Clin Res, 2024, 37(2): 246-252. |
| [1] | ZHOU Sifeng, ZHU Jieyun, XU Haishu, NI Ying. Advances in mechanism on pigment epithelium derived factor in diabetes retinopathy [J]. Journal of Diagnostics Concepts & Practice, 2024, 23(02): 192-201. |
| [2] | XIE Yaqiong, LIN Xiaoyi. Value of serum-free light chain assay in differential diagnosis and staging of nephropathy of various etiologies [J]. Journal of Diagnostics Concepts & Practice, 2023, 22(02): 166-171. |
| [3] | LIN Xia, GAO Chao, HUANG Pei, WANG Gang, LIN Guozhen, REN Rujing. Analysis of clinical and imaging manifestations in 8 patients with MOGAG and literature review [J]. Journal of Diagnostics Concepts & Practice, 2022, 21(05): 606-612. |
| [4] | RUAN Yufeng, HU Liping, CHEN Shirong, YIN Jun, SUN Jing. Investigation on mastery status of standardized diagnosis and treatment of Helicobacter pylori(Hp) infection in general practitioners in Pudong New Aera, Shanghai [J]. Journal of Diagnostics Concepts & Practice, 2022, 21(03): 399-404. |
| [5] | KANG Jianqiang, DONG Yangyang, YANG Ling, SONG Zhen, FAN Jiaying. Effect of Haemophilus influenzae colonizing lower respiratory tract on airway inflammation and its signaling pathway in asthmatic mice [J]. Journal of Diagnostics Concepts & Practice, 2020, 19(1): 44-49. |
| [6] | SHAO Dandan, FU Yang, LUO Qi, CHEN Jie, MA Jianfang, HUANG Lei. Serum uric acid and Parkinson disease: a population-based prospective study [J]. Journal of Diagnostics Concepts & Practice, 2020, 19(02): 139-144. |
| [7] | HOU Yanan, XUAN Liping, ZHAO Zhiyun, LI Mian, CHEN Yuhong, DAI Meng, XU Min, BI Yufang, WANG Weiqing, GAO Jinli. Epidemiological study on association of uric acid to creatinine ratio with metabolic syndrome in middle-aged and elderly populationin Shanghai [J]. Journal of Diagnostics Concepts & Practice, 2019, 18(1): 44-50. |
| [8] | SHAO Wentao, SUN Haidong, WANG Qihan, LIU Qian, JIANG Zhaoyan, GU Aihua. Animal and in vitro study on mechanism of berberine alleviating high cholesterol induced liver injury [J]. Journal of Diagnostics Concepts & Practice, 2018, 17(03): 311-317. |
| [9] | WANG Yanping, CHEN Yuanyuan, WU Liping, CHEN Yafen, YANG Ke, LIU Yan. Toll-like receptor 4 regulates the inflammation induced by lipids in smooth muscle cells [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(05): 504-509. |
| [10] | LIU Ling, ZHANG Chen, LI Mingxin, QIN Ximiao, HUANG Bihong, XUE Jun. Correlation of expression of MCP-1 on wall of radial artery with stenosis of cannulation site in arteriovenous fistula with buttonhole in hemodialysis patients [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(04): 394-398. |
| [11] | WANG Weiyi, ZHANG Yongping, YUAN Yaozong, WU Yunlin, CHEN Ping. Experimental study on effect of PIAS1 in regulating migration of macrophage and its mechanism [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(01): 60-65. |
| [12] | HE Jingjing, LIU Jingyao, ZHANG Yan, ZHAO Dongmei, ZHENG Zunrong. Diagnostic value of IELISA for human Brucella infection [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(01): 84-87. |
| [13] | MENG Jun, PENG Yibing, WANG Xuefeng, CHEN Ninan, ZHANG Dongqing. A study on correlation between multiple sclerosis and Epstein-Barr virus and IL-17/IL-23 [J]. Journal of Diagnostics Concepts & Practice, 2017, 16(01): 88-92. |
| [14] | MU Jinjin, YANG Kang, FENG Yulan, FU Yi. New silent cerebral infarction in patients with hypertensive intracerebral hemorrhage: related risk factors and prognosis [J]. Journal of Diagnostics Concepts & Practice, 2016, 15(05): 492-497. |
| [15] | . [J]. Journal of Diagnostics Concepts & Practice, 2016, 15(03): 226-230. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||