

诊断学理论与实践 ›› 2024, Vol. 23 ›› Issue (05): 467-473.doi: 10.16150/j.1671-2870.2024.05.002
李延兵
收稿日期:2024-08-23
接受日期:2024-10-08
出版日期:2024-10-25
发布日期:2025-02-25
LI Yanbing
Received:2024-08-23
Accepted:2024-10-08
Published:2024-10-25
Online:2025-02-25
摘要:
糖尿病是一种常见的慢性疾病,在全球范围内造成了重大的卫生经济负担。糖尿病具有高度异质性,准确诊断和分型是实现糖尿病标准化精准治疗、改善患者临床结局的前提。近期,美国糖尿病协会(American Diabetes Association, ADA)发布了2024年《糖尿病诊疗标准》。糖尿病诊断和分型章节结合当前的最新进展,对非典型糖尿病的鉴别诊断、不同类型糖尿病的筛查、诊断和随访等流程均提出了推荐意见。本文对该指南这一部分内容进行了解读,以期为我国内分泌领域医务人员进行糖尿病诊断、分型和个体化诊疗实践提供参考。
中图分类号:
李延兵. 2024年美国糖尿病学会《糖尿病诊疗标准》解读——糖尿病诊断和分型[J]. 诊断学理论与实践, 2024, 23(05): 467-473.
LI Yanbing. Interpretation of 2024 American Diabetes Association’s Standards of Care in Diabetes — diabetes diagnosis and classification[J]. Journal of Diagnostics Concepts & Practice, 2024, 23(05): 467-473.
图1
新诊断成人疑似1型糖尿病筛查流程图 1:没有单一临床特征可独立诊断1型糖尿病。2:谷氨酸脱羧酶是测定的主要抗体,如果其结果为阴性,后续应检测胰岛酪氨酸磷酸酶2和(或)锌转运体8。对于未接受过胰岛素治疗的个体,检测抗胰岛素抗体或许可能有用;对于年龄<35岁且无2型糖尿病或单基因糖尿病临床特征的患者,阴性结果不会改变1型糖尿病的诊断,因为5%~10%的1型糖尿病患者没有抗体。3:单基因糖尿病特征是指存在下列一种或多种特征,包括诊断时HbA1c<58 mmol/mol (<7.5%);父母一方患有糖尿病;具有特定单基因疾病的特征(如肾囊肿、部分脂肪营养不良、母系遗传性耳聋以及无肥胖的情况下重度胰岛素抵抗);以及单基因糖尿病预测模型评估患病风险>5%。4:C肽检测仅适用于接受胰岛素治疗的人。进食后5 h内的随机C肽伴血糖检测可代替标准C肽刺激试验。如果结果≥600 pmol/L (≥1.8 ng/mL),结果可靠;如果结果<600 pmol/L (<1.8 ng/mL)且血糖<4 mmol/L (<70 mg/dL),考虑禁食原因,可重复检测;对于水平极低的结果[<80 pmol/L(如<0.24 ng/mL)],无需重复检测。如果患者接受胰岛素治疗,则必须在胰岛素停用前检测C肽,以排除严重的胰岛素缺乏症。勿在高血糖急症发生后2周内检测C肽。5:2型糖尿病的特征包括BMI增加(≥25 kg/m2)、无体重减轻、无酮症酸中毒和高血糖症状不明显。鉴别价值稍低的特征包括非白种人、家族史、就诊前症状轻微且病程长、代谢综合征的特征、无自身免疫家族史。6:如果基因检测未证实为单基因糖尿病,即使分类不明确,也应作出治疗的临床决策。7:老年人应强烈考虑2型糖尿病。在某些情况下,可能需要检查胰腺或考虑其他类型的糖尿病。8:可能患有1型糖尿病但未接受胰岛素治疗的患者,需要仔细监测和教育,以便在血糖恶化的情况下可以迅速开始使用胰岛素。9:C肽介于200~600 pmol/L(0.6~1.8 ng/mL)多见于1型糖尿病或MODY,也可见于接受胰岛素治疗的2型糖尿病患者,尤其是正常/低BMI或病程较长的患者。
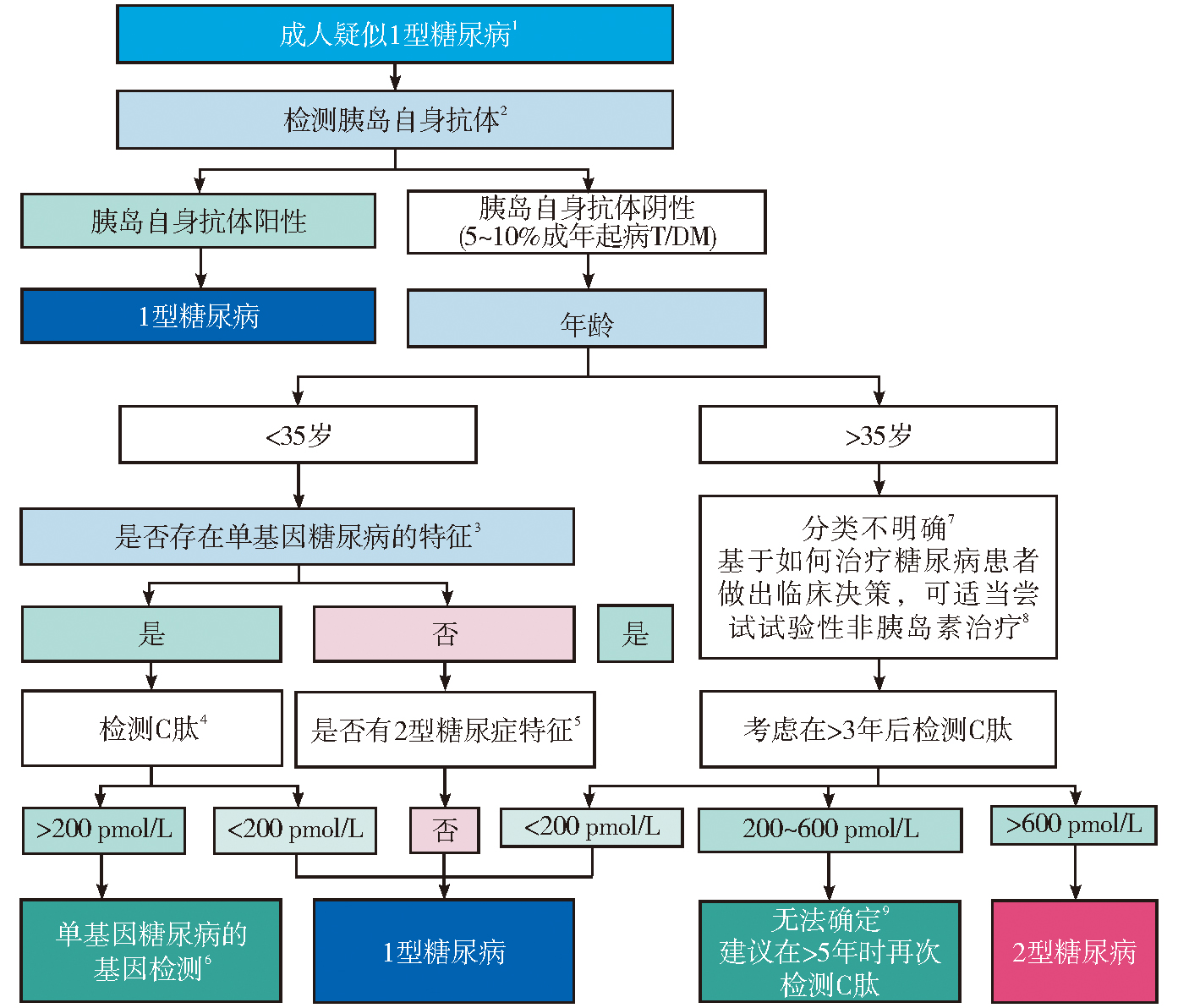
表3
无症状成人糖尿病或糖尿病前期筛查标准
| 筛查标准 |
|---|
| 对于有以下一种或多种风险因素的超重或肥胖成人(BMI≥25 kg/m2或亚裔美国人≥23 kg/m2),应考虑进行检测: · 糖尿病一级亲属 · 高危种族/族裔(例如,非洲裔美国人、拉丁美洲人、美洲原住民、亚裔美国人、太平洋岛民) · 心血管疾病史 · 高血压(≥130/80 mmHg或正在接受高血压治疗) · HDL胆固醇水平< 35 mg/dL (0.90 mmol/L)和/或甘油三酯水平> 250 mg/dL (2.82 mmol/L) · 多囊卵巢综合征女性 · 缺乏运动 · 与胰岛素抵抗相关的其他临床病症(例如严重肥胖、黑棘皮病) |
| 糖尿病前期(A1C ≥5.7%、IGT或IFG)的患者应每年检测一次 |
| 确诊为GDM的女性应至少每3年进行一次直至终生 |
| 对于所有其他患者,检测应在35岁时开始 |
| 如果结果正常,应至少每隔3年重复检测一次,并根据初始结 果和风险状态考虑缩短间隔 |
| · 艾滋病毒携带者、接触高危药物、胰腺炎病史 |
| [1] |
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in diabetes-2024[J]. Diabetes Care, 2024, 47(Suppl 1):S20-S42.
doi: 10.2337/dc24-S002 pmid: 38078589 |
| [2] | MEIJNIKMAN A S, DE BLOCK C E M, DIRINCK E, et al. Not performing an OGTT results in significant underdiagnosis of (pre)diabetes in a high risk adult Caucasian population[J]. Int J Obes (Lond), 2017, 41(11):1615-1620. |
| [3] |
HOLT R I G, DEVRIES J H, HESS-FISCHL A, et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)[J]. Diabetes Care, 2021, 44(11):2589-2625.
doi: 10.2337/dci21-0043 pmid: 34593612 |
| [4] |
INSEL R A, DUNNE J L, ATKINSON M A, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association[J]. Diabetes Care, 2015, 38(10):1964-1974.
doi: 10.2337/dc15-1419 pmid: 26404926 |
| [5] |
SOSENKO J M, PALMER J P, RAFKIN-MERVIS L, et al. Incident dysglycemia and progression to type 1 diabetes among participants in the Diabetes Prevention Trial-Type 1[J]. Diabetes Care, 2009, 32(9):1603-1607.
doi: 10.2337/dc08-2140 pmid: 19487644 |
| [6] | KRISCHER J P. Type 1 Diabetes Trialnet Study Group. The use of intermediate endpoints in the design of type 1 diabetes prevention trials[J]. Diabetologia, 2013, 56(9):1919-1924. |
| [7] |
SMITH C J, ALMODALLAL Y, JATOI A. Rare adverse events with programmed death-1 and programmed death-1 ligand inhibitors: justification and rationale for a systematic review[J]. Curr Oncol Rep, 2021, 23(7):86.
doi: 10.1007/s11912-021-01089-9 pmid: 34037893 |
| [8] |
ZHAO Z, WANG X, BAO X Q, et al. Autoimmune polyendocrine syndrome induced by immune checkpoint inhibitors: a systematic review[J]. Cancer Immunol Immunother, 2021, 70(6):1527-1540.
doi: 10.1007/s00262-020-02699-1 pmid: 33200250 |
| [9] |
CHEN X, AFFINATI AH, LEE Y, et al. Immune checkpoint inhibitors and risk of type 1 diabetes[J]. Diabetes Care, 2022, 45(5):1170-1176.
doi: 10.2337/dc21-2213 pmid: 35238899 |
| [10] |
ARSLANIAN S, BACHA F, GREY M, et al. Evaluation and management of youth-onset type 2 diabetes: a position statement by the american diabetes association[J]. Diabetes Care, 2018, 41(12):2648-2668.
doi: 10.2337/dci18-0052 pmid: 30425094 |
| [11] | MANSI I A, SUMITHRAN P, KINAAN M. Risk of diabetes with statins[J]. BMJ, 2023,381:e071727. |
| [12] | ECKHARDT B J, HOLZMAN R S, KWAN C K, et al. Glycated hemoglobin A(1c) as screening for diabetes mellitus in HIV-infected individuals[J]. AIDS Patient Care STDS, 2012, 26(4):197-201. |
| [13] | American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, et al. Consensus development conference on antipsychotic drugs and obesity and diabetes[J]. Diabetes Care, 2004, 27(2):596-601. |
| [14] |
EWALD N, BRETZEL R G. Diabetes mellitus secondary to pancreatic diseases (type 3c)--are we neglecting an important disease?[J] Eur J Intern Med, 2013, 24(3):203-206.
doi: 10.1016/j.ejim.2012.12.017 pmid: 23375619 |
| [15] | HARDT P D, BRENDEL M D, KLOER H U, et al. Is pancreatic diabetes (type 3c diabetes) underdiagnosed and misdiagnosed?[J] Diabetes Care, 2008,31 Suppl 2:S165-169. |
| [16] |
WOODMANSEY C, MCGOVERN A P, MCCULLOUGH K A, et al. Incidence, demographics, and clinical characteristics of diabetes of the exocrine pancreas (Type 3c): a retrospective cohort study[J]. Diabetes Care, 2017, 40(11):1486-1493.
doi: 10.2337/dc17-0542 pmid: 28860126 |
| [17] | PETROV M S, BASINA M. Diagnosis Of Endocrine Di-sease: diagnosing and classifying diabetes in diseases of the exocrine pancreas[J]. Eur J Endocrinol, 2021, 184(4):R151-R163. |
| [18] | MORAN A, PILLAY K, BECKER D, et al. ISPAD clinical practice consensus guidelines 2018: management of cystic fibrosis-related diabetes in children and adolescents[J]. Pediatr Diabetes, 2018,19 Suppl 27:64-74. |
| [19] | DARUKHANAVALA A, VAN DESSEL F, HO J, et al. Use of hemoglobin A1c to identify dysglycemia in cystic fibrosis[J]. PLoS One, 2021, 16(4):e0250036. |
| [20] |
SHARIF A, HECKING M, DE VRIES A P, et al. Proceedings from an international consensus meeting on posttransplantation diabetes mellitus: recommendations and future directions[J]. Am J Transplant, 2014, 14(9):1992-2000.
doi: 10.1111/ajt.12850 pmid: 25307034 |
| [21] |
GULSOY KIRNAP N, BOZKUS Y, HABERAL M. Analysis of risk factors for posttransplant diabetes mellitus after kidney transplantation: single-center experience[J]. Exp Clin Transplant, 2020, 18(Suppl 1):36-40.
doi: 10.6002/ect.TOND-TDTD2019.O8 pmid: 32008491 |
| [22] |
SHARIF A, MOORE R H, BABOOLAL K. The use of oral glucose tolerance tests to risk stratify for new-onset diabetes after transplantation: an underdiagnosed phenomenon[J]. Transplantation, 2006, 82(12):1667-1672.
doi: 10.1097/01.tp.0000250924.99855.42 pmid: 17198257 |
| [23] | HECKING M, WERZOWA J, HAIDINGER M, et al. Novel views on new-onset diabetes after transplantation: development, prevention and treatment[J]. Nephrol Dial Transplant, 2013, 28(3):550-566. |
| [24] |
DE FRANCO E, FLANAGAN S E, HOUGHTON J A, et al. The effect of early, comprehensive genomic testing on clinical care in neonatal diabetes: an international cohort study[J]. Lancet, 2015, 386(9997):957-963.
doi: 10.1016/S0140-6736(15)60098-8 pmid: 26231457 |
| [25] |
TIMSIT J, SAINT-MARTIN C, DUBOIS-LAFORGUE D, et al. Searching for Maturity-onset diabetes of the young (MODY): when and what for?[J] Can J Diabetes, 2016, 40(5):455-461.
doi: S1499-2671(15)30008-3 pmid: 27103109 |
| [26] | AWA W L, SCHOBER E, WIEGAND S, et al. Reclassification of diabetes type in pediatric patients initially classified as type 2 diabetes mellitus: 15 years follow-up usi-ng routine data from the German/Austrian DPV database[J]. Diabetes Res Clin Pract, 2011, 94(3):463-467. |
| [27] |
SHIELDS B M, HICKS S, SHEPHERD M H, et al. Maturity-onset diabetes of the young (MODY): how many cases are we missing?[J] Diabetologia, 2010, 53(12):2504-2508.
doi: 10.1007/s00125-010-1799-4 pmid: 20499044 |
| [28] | RUBIO-CABEZAS O, HATTERSLEY A T, NJØLSTAD P R, et al. ISPAD clinical practice consensus guidelines 2014. The diagnosis and management of monogenic diabetes in children and adolescents[J]. Pediatr Diabetes, 2014,15 Suppl 20:47-64. |
| [29] |
ZHANG X, GREGG E W, WILLIAMSON D F, et al. A1C level and future risk of diabetes: a systematic review[J]. Diabetes Care, 2010, 33(7):1665-1673.
doi: 10.2337/dc09-1939 pmid: 20587727 |
| [30] | BUCHANAN T A, XIANG A, KJOS S L, et al. What is gestational diabetes?[J] Diabetes Care, 2007,30 Suppl 2:S105-111. |
| [31] | VOUNZOULAKI E, KHUNTI K, ABNER S C, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis[J]. BMJ, 2020,369:m1361. |
| [32] | World Health Organization. Classification of diabetes mellitus[M]. Geneva: World Health Organization, 2019. |
| [33] | 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志, 2021, 13(4):315-409. |
| Chinese Diabetes Society. Chinese guidelines for the prevention and treatment of type 2 diabetes (2020 edition)[J]. Chin J Diabetes Mellitus, 2021, 13(4):315-409. | |
| [34] | Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus[J]. Diabetes Care, 2003,26 Suppl 1:S5-20. |
| [35] | BERGMAN M, MANCO M, SATMAN I, et al. International diabetes federation position statement on the 1-hour post-load plasma glucose for the diagnosis of intermediate hyperglycaemia and type 2 diabetes[J]. Diabetes Res Clin Pract, 2024,209:111589. |
| [1] | 黄敏, 左莹. 以低钾血症首发症状的原发性干燥综合征致I型肾小管酸中毒1例报道[J]. 诊断学理论与实践, 2024, 23(06): 624-627. |
| [2] | 裴舟, 罗飞宏. 中国儿童糖尿病诊治进展[J]. 诊断学理论与实践, 2024, 23(05): 461-466. |
| [3] | 于津, 汪杰, 王虎军, 王丛笑, 李瑛琦, 方伯言, 王颖鹏. 基于机器学习的功能性近红外光谱信号识别早期帕金森病患者的研究[J]. 诊断学理论与实践, 2024, 23(05): 484-493. |
| [4] | 钱玲玲, 裴孝平, 孙爱红, 何斌, 孙梅. 单中心7例获得性血友病A的回顾性临床研究[J]. 诊断学理论与实践, 2024, 23(05): 524-530. |
| [5] | 高泉澄, 黄慧. 肿瘤诱导血小板在临床常见肿瘤诊断中的应用研究进展[J]. 诊断学理论与实践, 2024, 23(05): 550-556. |
| [6] | 李静, 单忠艳. 我国甲状腺功能亢进的诊治现状及挑战[J]. 诊断学理论与实践, 2024, 23(04): 347-353. |
| [7] | 周建桥, 张璐, 徐上妍. 中国甲状腺结节超声诊治现状及挑战[J]. 诊断学理论与实践, 2024, 23(04): 362-370. |
| [8] | 伏秋燚, 展颖, 谭令, 朱宏, 朱乃懿, 孙琨, 柴丽, 柴维敏. 全野数字乳腺X线摄影及联合数字乳腺断层合成X线摄影在乳腺癌诊断中效能评价[J]. 诊断学理论与实践, 2024, 23(04): 385-391. |
| [9] | 李卓含, 黄新韵, 郭睿, 李彪. 18F-FDG PET/CT在滤泡性淋巴瘤诊断和预后评估中的研究进展[J]. 诊断学理论与实践, 2024, 23(04): 439-444. |
| [10] | 张天翼, 严福华. 能量CT虚拟单能量图像与碘图在腹部实质性脏器疾病诊断中的应用进展[J]. 诊断学理论与实践, 2024, 23(04): 452-456. |
| [11] | 丁宁, 刘琳, 金佩佩, 王芳, 王天凯. 网织红细胞平均血红蛋白含量在缺铁性贫血及其严重程度的诊断效能分析[J]. 诊断学理论与实践, 2024, 23(03): 318-323. |
| [12] | 中国老年医学学会血液学分会MDS专委会. 中国老年骨髓增生异常性肿瘤诊断和治疗专家共识(2024版)[J]. 诊断学理论与实践, 2024, 23(03): 285-296. |
| [13] | 王刚, 齐金蕾, 刘馨雅, 任汝静, 林绍慧, 胡以松, 李海霞, 谢心怡, 王金涛, 李建平, 朱怡康, 高梦伊, 杨竣杰, 王怡然, 井玉荣, 耿介立, 支楠, 曹雯炜, 徐群, 余小萍, 朱圆, 周滢, 王琳, 高超, 李彬寅, 陈生弟, 袁芳, 窦荣花, 刘晓云, 李雪娜, 尹雅芙, 常燕, 徐刚, 辛佳蔚, 钟燕婷, 李春波, 王颖, 周脉耕, 陈晓春, 代表中国阿尔茨海默病报告编写组. 中国阿尔茨海默病报告2024[J]. 诊断学理论与实践, 2024, 23(03): 219-256. |
| [14] | 缪婕, 王巍, 赵雅洁, 张凤如, 沈琳辉. 老年男性2型糖尿病患者游离三碘甲状腺原氨酸水平与左心室舒张功能不全相关[J]. 诊断学理论与实践, 2024, 23(02): 155-161. |
| [15] | 高梦, 柴维敏, 严福华. 胰腺囊性肿瘤的CT/MRI诊断进展[J]. 诊断学理论与实践, 2024, 23(02): 184-191. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||