

诊断学理论与实践 ›› 2023, Vol. 22 ›› Issue (05): 429-440.doi: 10.16150/j.1671-2870.2023.05.003
收稿日期:2023-10-23
出版日期:2023-10-25
发布日期:2024-03-15
通讯作者:
王书奎 E-mail: 基金资助:
QIN Xiaodan, SUN Huiling, PAN Bei, PAN Yuqin, WANG Shukui( )
)
Received:2023-10-23
Online:2023-10-25
Published:2024-03-15
摘要:
目的:探讨微小RNA(microRNA, miRNA)在结直肠癌(colorectal cancer, CRC)疾病进展中的作用及临床应用价值。方法:基于TCGA数据库,筛选分析人类结肠癌及癌旁组织的转录组差异表达miRNA,以miRNA-1229-3p作为研究对象,在GEO数据库与Starbase数据库中验证其表达水平。采用生物信息学方法对miR-1229-3p的生物功能特征进行分析,构建miR-1229-3p过表达细胞系及miR-1229-3p敲降细胞系,通过CCK-8实验、克隆形成实验、EdU实验、Transwell实验、流式细胞术实验在体外探究miR-1229-3p对CRC细胞增殖、转移、凋亡的影响,并通过裸鼠移植瘤试验探究miR-1229-3p对CRC细胞体内增殖的影响。通过DIANA 、TargetScan、miRDB数据库筛选miR-1229-3p的靶基因,并通过KEGG富集分析、GO分析靶基因的生物学功能。检测60例CRC患者及60例健康体检者血浆外泌体中的miR-1229-3p含量,采用受试者工作特征曲线(receiver operating characteristic curve, ROC)分析其对CRC患者的诊断效能。结果:数据分析显示,miR-1229-3p在CRC细胞和组织中表达下调。生物信息学方法预测结果显示,miR-1229-3p与肿瘤的进展途径(如上皮间质转化、血管形成等)呈显著负相关(R<0,P<0.05)。体内、外研究表明,过表达miR-1229-3p后,CRC细胞的增殖、迁移和侵袭能力受到抑制,且其潜在靶基因SETD7在细胞中的表达下调;而敲低miR-1229-3p后可抑制CRC细胞的凋亡。CRC患者血浆外泌体中的miR-1229-3p含量较健康体检者降低,ROC曲线分析显示,miR-1229-3p诊断CRC的约登指数最大值为0.586 8,曲线下面积为0.863 2(P<0.01)。结论:miR-1229-3p在CRC中表达下调,SETD7是其潜在的靶基因,miR-1229-3p可抑制CRC细胞增殖、迁移与侵袭,促进CRC细胞凋亡,有望作为诊断CRC的潜在生物标志物。
中图分类号:
秦晓丹, 孙慧玲, 潘蓓, 潘玉琴, 王书奎. miR-1229-3p抑制结直肠癌疾病进展及作为潜在生物标志物的研究[J]. 诊断学理论与实践, 2023, 22(05): 429-440.
QIN Xiaodan, SUN Huiling, PAN Bei, PAN Yuqin, WANG Shukui. miR-1229-3p inhibits the malignant progression of colorectal cancer and serves as a potential biomarker[J]. Journal of Diagnostics Concepts & Practice, 2023, 22(05): 429-440.

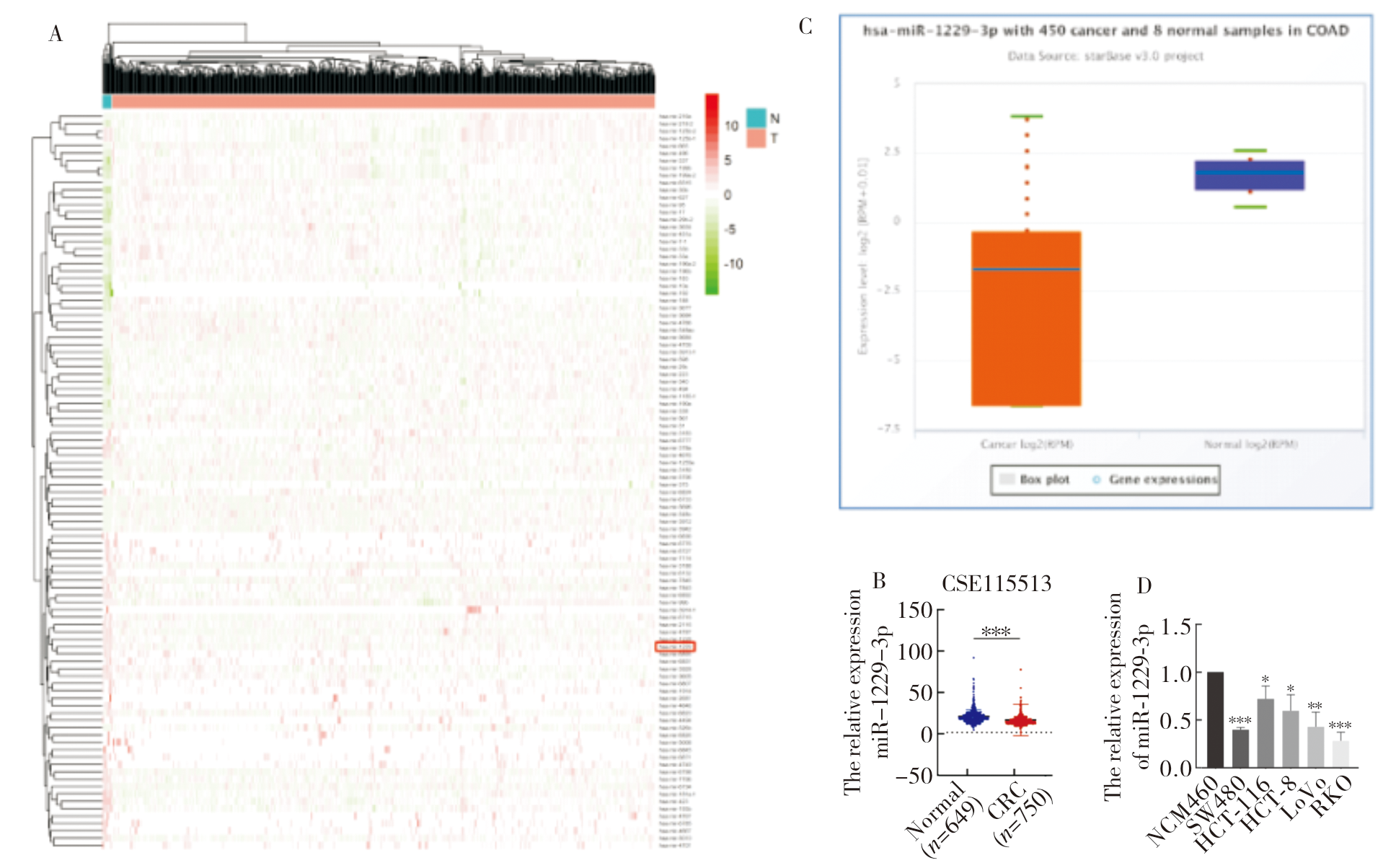
图1
miR-1229-3p在人类CRC细胞中表达下调 A:来源于TCGA数据库中CRC及其相应正常组织的RNA测序数据生成的差异表达miRNA的分层聚类热图。热图中的红色表示上调;绿色表示下调。红线表示miR-1229-3p;B:miR-1229-3p在GSE115513数据集中的表达水平(正常组织649例,肿瘤组织750例);C:Starbase数据库中,450例CRC患者组织及8例正常组织中miR-1229-3p的表达水平;D: qRT-PCR 检测人CRC细胞系与人正常肠上皮细胞株NCM460中miR-1229-3p的表达水平。*:P<0.05; **:P<0.01; ***:P<0.001。
| [1] |
SIEGEL R L, MILLER K D, WAGLE N S, et al. Cancer statistics, 2023[J]. CA Cancer J Clin, 2023, 73(1):17-48.
doi: 10.3322/caac.v73.1 URL |
| [2] | 中华人民共和国国家卫生健康委员会. 中国结直肠癌诊疗规范(2023版)[J]. 中华消化外科杂志, 2023, 22(6):667-698. |
| National Health Commission of the People′s Republic of China. Chinese protocol of diagnosis and treatment of colorectal cancer (2023 edition)[J]. Chin J Dig Surg, 2023, 22(6):667-698. | |
| [3] |
SUNG H, FERLAY J, SIEGEL R L, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3):209-249.
doi: 10.3322/caac.v71.3 URL |
| [4] |
ALLEMANI C, MATSUDA T, DI CARLO V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries[J]. Lancet, 2018, 391(10125):1023-1075.
doi: S0140-6736(17)33326-3 pmid: 29395269 |
| [5] | 张忠涛. 中国结直肠外科20年回顾与展望[J]. 中华消化外科杂志, 2022, 21(01):53-56. |
| ZHANG Z T. Two-decade retrospect and prospect of colorectal surgery in China[J]. Chin J Dig Surg, 2022, 21(1):53-56. | |
| [6] | 杨盈, 孟文建, 王自强. 结直肠癌的综合治疗[J]. 中华消化外科杂志, 2022, 21(06):753-765. |
| YANG Ying, MENG Wenjian, WANG Ziqiang. Comprehensive treatment of colorectal cancer[J]. Chin J Dig Surg, 2022, 21(06):753-765. | |
| [7] |
HARRIS T J, MCCORMICK F. The molecular pathology of cancer[J]. Nat Rev Clin Oncol, 2010, 7(5):251-265.
doi: 10.1038/nrclinonc.2010.41 pmid: 20351699 |
| [8] |
AMBROS V, BARTEL B, BARTEL D P, et al. A uniform system for microRNA annotation[J]. RNA, 2003, 9(3):277-279.
pmid: 12592000 |
| [9] |
POY M N, ELIASSON L, KRUTZFELDT J, et al. A pancreatic islet-specific microRNA regulates insulin secretion[J]. Nature, 2004, 432(7014):226-230.
doi: 10.1038/nature03076 |
| [10] |
CALAME K. MicroRNA-155 function in B Cells[J]. Immunity, 2007, 27(6):825-827.
doi: 10.1016/j.immuni.2007.11.010 pmid: 18093533 |
| [11] |
GRECO S J, RAMESHWAR P. MicroRNAs regulate synthesis of the neurotransmitter substance P in human me-senchymal stem cell-derived neuronal cells[J]. Proc Natl Acad Sci U S A, 2007, 104(39):15484-15489.
doi: 10.1073/pnas.0703037104 URL |
| [12] |
STEPONAITIENE R, KUPCINSKAS J, LANGNER C, et al. Epigenetic silencing of miR-137 is a frequent event in gastric carcinogenesis[J]. Mol Carcinog, 2016, 55(4):376-386.
doi: 10.1002/mc.22287 URL |
| [13] |
WANG F, YING H Q, HE B S, et al. Upregulated lncRNA-UCA1 contributes to progression of hepatocellular carcinoma through inhibition of miR-216b and activation of FGFR1/ERK signaling pathway[J]. Oncotarget, 2015, 6(10):7899-7917.
doi: 10.18632/oncotarget.3219 pmid: 25760077 |
| [14] |
LIU R, GU J, JIANG P, et al. DNMT1-microRNA126 epigenetic circuit contributes to esophageal squamous cell carcinoma growth via ADAM9-EGFR-AKT signaling[J]. Clin Cancer Res, 2015, 21(4):854-863.
doi: 10.1158/1078-0432.CCR-14-1740 pmid: 25512445 |
| [15] |
LEE Y S, DUTTA A. MicroRNAs in cancer[J]. Annu Rev Pathol, 2009, 4:199-227.
doi: 10.1146/annurev.pathol.4.110807.092222 pmid: 18817506 |
| [16] |
GILLIES J K, LORIMER I A. Regulation of p27Kip1 by miRNA 221/222 in glioblastoma[J]. Cell Cycle, 2007, 6(16):2005-2009.
doi: 10.4161/cc.6.16.4526 pmid: 17721077 |
| [17] |
JOHNSON C D, ESQUELA-KERSCHER A, STEFANI G, et al. The let-7 microRNA represses cell proliferation pathways in human cells[J]. Cancer Res, 2007, 67(16):7713-7722.
doi: 10.1158/0008-5472.CAN-07-1083 pmid: 17699775 |
| [18] |
MOTT J L, KOBAYASHI S, BRONK S F, et al. mir-29 regulates Mcl-1 protein expression and apoptosis[J]. Oncogene, 2007, 26(42):6133-6140.
pmid: 17404574 |
| [19] |
BOMMER G T, GERIN I, FENG Y, et al. p53-mediated activation of miRNA34 candidate tumor-suppressor genes[J]. Curr Biol, 2007, 17(15):1298-1307.
doi: 10.1016/j.cub.2007.06.068 pmid: 17656095 |
| [20] |
SCOTT G K, GOGA A, BHAUMIK D, et al. Coordinate suppression of ERBB2 and ERBB3 by enforced expression of micro-RNA miR-125a or miR-125b[J]. J Biol Chem, 2007, 282(2):1479-1486.
doi: 10.1074/jbc.M609383200 pmid: 17110380 |
| [21] |
KUMAR M S, LU J, MERCER K L, et al. Impaired microRNA processing enhances cellular transformation and tumorigenesis[J]. Nat Genet, 2007, 39(5):673-677.
doi: 10.1038/ng2003 pmid: 17401365 |
| [22] |
JUNG G, HERNÁNDEZ-ILLÁN E, MOREIRA L, et al. Epigenetics of colorectal cancer: biomarker and therapeutic potential[J]. Nat Rev Gastroenterol Hepatol, 2020, 17(2):111-130.
doi: 10.1038/s41575-019-0230-y pmid: 31900466 |
| [23] |
FARHAN M, WANG H, GAUR U, et al. FOXO signaling pathways as therapeutic targets in cancer[J]. Int J Biol Sci, 2017, 13(7):815-827.
doi: 10.7150/ijbs.20052 pmid: 28808415 |
| [24] |
OUDHOFF M J, BRAAM M J S, FREEMAN S A, et al. SETD7 controls intestinal regeneration and tumorigene-sis by regulating Wnt/β-Catenin and Hippo/YAP signa-ling[J]. Dev Cell, 2016, 37(1):47-57.
doi: 10.1016/j.devcel.2016.03.002 URL |
| [25] |
DEWS M, HOMAYOUNI A, YU D, et al. Augmentation of tumor angiogenesis by a Myc-activated microRNA cluster[J]. Nat Genet, 2006, 38(9):1060-1065.
doi: 10.1038/ng1855 pmid: 16878133 |
| [26] |
MERTENS-TALCOTT S U, CHINTHARLAPALLI S, LI X, et al. The oncogenic microRNA-27a targets genes that regulate specificity protein transcription factors and the G2-M checkpoint in MDA-MB-231 breast cancer cells[J]. Cancer Res, 2007, 67(22):11001-110011.
doi: 10.1158/0008-5472.CAN-07-2416 URL |
| [27] |
HOU Y, ZHANG Q, PANG W, et al. YTHDC1-mediated augmentation of miR-30d in repressing pancreatic tumorigenesis via attenuation of RUNX1-induced transcriptional activation of Warburg effect[J]. Cell Death Differ, 2021, 28(11):3105-3124.
doi: 10.1038/s41418-021-00804-0 pmid: 34021267 |
| [28] |
KONOSHENKO M Y, BRYZGUNOVA O E, LAKTIONOV P P. miRNAs and androgen deprivation therapy for prostate cancer[J]. Biochim Biophys Acta Rev Cancer, 2021, 1876(2):188625.
doi: 10.1016/j.bbcan.2021.188625 URL |
| [29] |
HU X, CHEN Q, GUO H, et al. Identification of target PTEN-based miR-425 and miR-576 as potential diagnostic and immunotherapeutic biomarkers of colorectal cancer with liver metastasis[J]. Front Oncol, 2021, 11:657984.
doi: 10.3389/fonc.2021.657984 URL |
| [30] |
LONE W, BOUSKA A, SHARMA S, et al. Genome-wide miRNA expression profiling of molecular subgroups of peripheral T-cell lymphoma[J]. Clin Cancer Res, 2021, 27(21):6039-6053.
doi: 10.1158/1078-0432.CCR-21-0573 URL |
| [31] |
KONISHI H, SATO H, TAKAHASHI K, et al. Tumor-progressive mechanisms mediating miRNA-protein interaction[J]. Int J Mol Sci, 2021, 22(22):12303.
doi: 10.3390/ijms222212303 URL |
| [32] |
BUTKYTĖ S, ČIUPAS L, JAKUBAUSKIENĖ E, et al. Splicing-dependent expression of microRNAs of mirtron origin in human digestive and excretory system cancer cells[J]. Clin Epigenetics, 2016, 8:33.
doi: 10.1186/s13148-016-0200-y pmid: 27019673 |
| [33] |
NISHIBEPPU K, KOMATSU S, IMAMURA T, et al. Plasma microRNA profiles: identification of miR-1229-3p as a novel chemoresistant and prognostic biomarker in gastric cancer[J]. Sci Rep, 2020, 10(1):3161.
doi: 10.1038/s41598-020-59939-8 pmid: 32081926 |
| [34] |
ZHAO X, CUI L. A robust six-miRNA prognostic signature for head and neck squamous cell carcinoma[J]. J Cell Physiol, 2020, 235(11):8799-8811.
doi: 10.1002/jcp.29723 pmid: 32342519 |
| [35] |
ZHANG C, ZHANG Q, LI H, et al. miR-1229-3p as a prognostic predictor facilitates cell viability, migration, and invasion of hepatocellular carcinoma[J]. Horm Metab Res, 2021, 53(11):759-766.
doi: 10.1055/a-1646-8415 pmid: 34740278 |
| [36] | CAO L, WANG M, XU K. Research progress of role and mechanism of SETD7 in tumor occurrence and progression[J]. Zhongguo Fei Ai Za Zhi, 2023, 26(1):38-45. |
| [1] | 常宇宸, 李京波. 心肌梗死中铁死亡标志物研究进展[J]. 诊断学理论与实践, 2023, 22(02): 197-202. |
| [2] | 陈国群, 蔡姣迪. 2022年美国国立综合癌症网络(NCCN)《非小细胞肺癌临床诊疗指南》(第4版及第5版)解读[J]. 诊断学理论与实践, 2023, 22(01): 8-13. |
| [3] | 李佳曦, 汪锦江, 俞立萍, 袁英, 乔光磊, 马俐君. RAB25沉默抑制结直肠癌细胞铁死亡的作用研究[J]. 诊断学理论与实践, 2022, 21(06): 710-718. |
| [4] | 武冬冬, 陈玉辉, 刘芳, 刘银红, 蒋景文. 脑小血管疾病合并中枢神经系统退行性疾病机制的研究进展[J]. 诊断学理论与实践, 2022, 21(05): 644-649. |
| [5] | 杨蕊馨, 杜宇童, 燕然林, 朱正纲, 李琛, 于颖彦. 消化道肿瘤单细胞转录组测序研究中生物样本前处理改良的探索[J]. 诊断学理论与实践, 2022, 21(05): 567-574. |
| [6] | 周思锋, 徐海舒, 范欣生. 基于不同生物样本代谢组学的OSAHS生物标志物研究进展[J]. 诊断学理论与实践, 2022, 21(04): 535-540. |
| [7] | 倪瀚文, 吴立群. 外泌体在心肌缺血及房颤诊治中的应用前景研究进展[J]. 诊断学理论与实践, 2020, 19(02): 199-202. |
| [8] | 陈海燕, 杨小宝, 许大康. 新生物标志物在胃肠道肿瘤中疗效预测和预后价值的研究进展[J]. 诊断学理论与实践, 2019, 18(06): 704-710. |
| [9] | 罗清琼, 陈福祥. 肿瘤免疫治疗策略的转变及相关标志物研究现状[J]. 诊断学理论与实践, 2019, 18(04): 387-393. |
| [10] | 杜坤, 杨喜, 卞炳贤, 任懿倩, 张广慧. 血清presepsin(sCD14-ST)、降钙素原、C反应蛋白和白介细胞素-6诊断血流细菌感染的诊断性能比较[J]. 诊断学理论与实践, 2018, 17(05): 581-585. |
| [11] | 崔诗爽, 陈生弟, 王刚. 帕金森病体液生物标志物研究进展[J]. 诊断学理论与实践, 2018, 17(04): 471-476. |
| [12] | 娄加陶, 张宸梓. 外泌体的检测及临床应用[J]. 诊断学理论与实践, 2018, 17(02): 141-146. |
| [13] | 牟姗, 陈哲君, 谢园园. 生物标志物在肾脏损伤诊断中的临床应用[J]. 诊断学理论与实践, 2017, 16(04): 358-362. |
| [14] | 商慧芳, 陈永平,. 帕金森病生物标志物的研究现状及展望[J]. 诊断学理论与实践, 2016, 15(02): 92-95. |
| [15] | 张月琪, 任汝静, 王刚,. 尿液生物标志物对痴呆诊断价值的研究进展[J]. 诊断学理论与实践, 2016, 15(02): 190-194. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||